Category: Parkinson's Disease: Neuroimaging
Objective: We aimed to assess changes in brain functional networks and accompanying symptoms over years in patients with idiopathic rapid eye movement sleep behavior disorder (iRBD), preceding synucleinopathies.
Background: Resting-state functional connectivity magnetic resonance imaging (rsfcMRI) may provide an imaging marker for the early diagnosis of synucleinopathy [1], considering already many reports indicating abnormal functional connectivities (FCs) in iRBD [2-4]. However, prior neuroimaging studies of iRBD have limitations in terms of sample size, correlation with clinical symptoms, and longitudinal changes.
Method: The Japan Parkinson’s Progressive Markers Initiative (J-PPMI) study has acquired longitudinal data from polysomnography-confirmed patients with iRBD at five centers. Ninety-seven patients (mean age 71.9 ± 5.3 (standard deviation) years at the baseline; 72 males) underwent rsfcMRI and neurological evaluations annually over five years (57 patients had finished the 5th visit). A region-of-interest analysis was performed using a functional connectivity toolbox. Alterations of FCs were evaluated by a repeated measures analysis of variance (RM-ANOVA) design, using the threshold at p = 0.05 (familywise error corrected) with the threshold-free cluster enhancement method. A correlation analysis was conducted between clinical indices and the first principal component characterizing each brain network, acquired through a principal component analysis (PCA) of rsfcMRI data at the final visit.
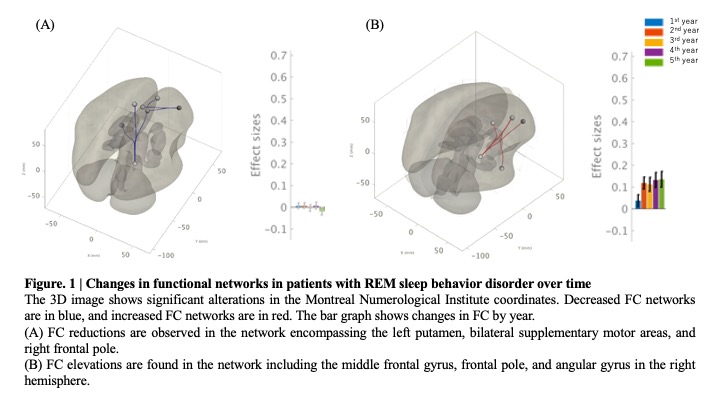
Results: Results: RM-ANOVA detected longitudinal changes of FCs in multiple brain networks. We found the FC-reductions in the motor network involving the left putamen, bilateral supplementary motor areas, and the right frontal pole (p < 0.001) [Figure 1 (A)]. The correlation analysis revealed a weak correlation between the 1st PCA component of this network with PD motor symptoms. We also found the elevation of FCs in the cognitive network involving the middle frontal gyrus, the frontal pole, and the angular gyrus in the right hemisphere (p = 0.006) [Figure 1 (B)]. A weak negative correlation was found between the 1st PCA component of this network and a global cognitive function.
Conclusion: Patients with iRBD, most of them would develop synucleinopathy in due course, showed abnormality in both motor and cognitive networks overtime, yet with differential temporal patterns.
References: [1] Hohenfeld, C., Werner, C. J., & Reetz, K. (2018). Resting-state connectivity in neurodegenerative disorders: Is there potential for an imaging biomarker? NeuroImage: Clinical, 18(November 2017), 849–870. https://doi.org/10.1016/j.nicl.2018.03.013
[2] Rolinski, M., Griffanti, L., Piccini, P., Roussakis, A. A., Szewczyk-Krolikowski, K., Menke, R. A., Quinnell, T., Zaiwalla, Z., Klein, J. C., Mackay, C. E., & Hu, M. T. M. (2016). Basal ganglia dysfunction in idiopathic REM sleep behaviour disorder parallels that in early Parkinson’s disease. Brain, 139(8), 2224–2234. https://doi.org/10.1093/brain/aww124
[3] Valli, M., Uribe, C., Mihaescu, A., & Strafella, A. P. (2022). Neuroimaging of rapid eye movement sleep behavior disorder and its relation to Parkinson’s disease. In Journal of Neuroscience Research (Vol. 100, Issue 10, pp. 1815–1833). John Wiley and Sons Inc. https://doi.org/10.1002/jnr.25099
[4] Wakasugi, N., Togo, H., Mukai, Y., Nishikawa, N., Sakamoto, T., Murata, M., Takahashi, Y., Matsuda, H., & Hanakawa, T. (2021). Prefrontal network dysfunctions in rapid eye movement sleep behavior disorder. Parkinsonism and Related Disorders, 85(September 2020), 72–77. https://doi.org/10.1016/j.parkreldis.2021.03.005
To cite this abstract in AMA style:
N. Wakasugi, T. Takamura, M. Abe, Y. Mukai, N. Nishikawa, T. Hatano, Y. Shimo, K. Ikenaka, H. Kadotani, Y. Sumi, N. Sawamoto, H. Watanabe, H. Mochizuki, N. Hattori, M. Katsuno, Y. Takahashi, R. Takahashi, T. Hanakawa. Longitudinal changes in brain networks associated with clinical symptoms in idiopathic rapid eye movement sleep behavior disorder [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/longitudinal-changes-in-brain-networks-associated-with-clinical-symptoms-in-idiopathic-rapid-eye-movement-sleep-behavior-disorder/. Accessed April 26, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/longitudinal-changes-in-brain-networks-associated-with-clinical-symptoms-in-idiopathic-rapid-eye-movement-sleep-behavior-disorder/