Objective: To evaluate long-term effects of DBS in an international cohort of people with VPS16-related dystonia.
Background: Variants in VPS16 gene have recently been related to early onset segmental or generalized dystonia. Although good response to deep brain stimulation (DBS) in several subjects with VPS16-related dystonia has been reported, a formal evaluation of DBS effects in a larger cohort of patients has not been performed yet.
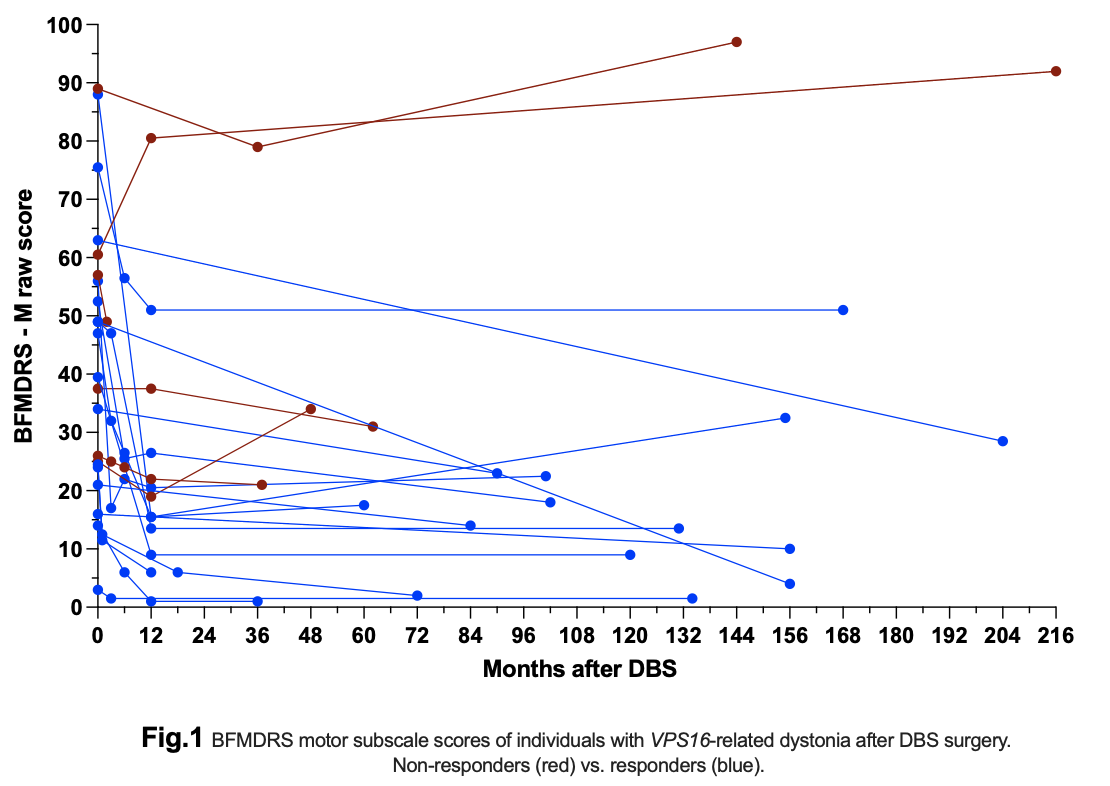
Method: In this retrospective observational study, preoperative and postoperative clinical data of VPS16-related dystonia patients who underwent GPi-DBS (one with additional VIM DBS) were collected from eight international centers. Demographic and clinical characteristics of dystonia, DBS parameters of stimulation and side effects, were collected at baseline, at 3, 6, 12 months and at last available follow-up after DBS. Motor symptoms and disability outcomes were assessed using the Burke-Fahn-Marsden Dystonia Rating Scale Motor (BFMDRS-M) and Disability (BFMDRS-D) Scale. The cut-off for responders to DBS was defined as ≥30% improvement in BFMDRS-M at last follow-up compared to baseline.
Results: Fourteen (63.6%) of the 22 included subjects were men. Age at dystonia onset and at time of surgery was 17.0±9.3 and 35.5±15.2 years, respectively. Disease duration at surgery was 18.5±9.7 years. Postoperative follow-up was 104.1±59.6 months (range 2-216). At last follow-up, compared to baseline, the BFMDRS-M and BFMDRS-D improvement was 43.0±39.3% (range -52.1 – 92.9%, [see Fig.1]) and 33.4±43.4% (21/22, range -42.9 – 100%), respectively. 16/22 subjects were considered as responders of whom twelve had ≥50% BFMDRS-M improvement. At last follow-up, significant negative relationship was observed between improvement of the BFMDRS-M and spasticity (p=0.003), as well as fixed skeletal problems (p=0.004). Of the six non-responders, only one did not improve at all after DBS, two improved temporarily, and three improved <30% in BFMDRS-M at last follow-up. Non-responders had a younger age of onset, younger age at DBS implantation, shorter disease duration at DBS surgery, and higher baseline BFMDRS scores compared to responders.
Conclusion: Bilateral pallidal DBS is an efficient treatment in about two thirds of patients with medically refractory and functionally disabling VPS16-related dystonia in the long-term follow-up.
To cite this abstract in AMA style:
T. Svorenova, LM. Romito, E. Mulroy, L. Cif, E. Moro, KE. Zeuner, S. Zittel, JN. Petry-Schmelzer, M. Ostrozovicova, V. Han, V. Magocova, K. Knorovsky, A. Kollova, B. Garavaglia, N. Golfrè-Andreasi, C. Reale, A. Mazzoni, A. Kaymak, G. Zorzi, R. Eleopra, V. Levi, T. Foltynie, P. Limousin, H. Akram, L. Zrinzo, F. Magrinelli, D. Murphy, H. Houlden, MA. Kurian, C. Baiata, S. Paschen, K. Lohmann, J. Volkmann, W. Hamel, MT. Barbe, R. Jech, P. Havrankova, J. Winkelmann, M. Zech, M. Skorvanek. Long-term outcomes of deep brain stimulation for VPS16-related dystonia: A multi-center international study [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/long-term-outcomes-of-deep-brain-stimulation-for-vps16-related-dystonia-a-multi-center-international-study/. Accessed December 31, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/long-term-outcomes-of-deep-brain-stimulation-for-vps16-related-dystonia-a-multi-center-international-study/