Objective: To determine the prevalence of risk of undiagnosed depression among people living with Parkinson’s disease (PwP) without a prior depression diagnosis.
Background: Parkinson’s disease (PD) is predominantly recognized by its motor symptoms, however, research on non-motor symptoms, including depression, remains ongoing [1]. Depression often coexists with PD, affecting 20 to 50% of PwP and potentially preceding motor symptoms [2]. This comorbidity negatively impacts the quality of life, treatment response, and caregiver burden. Despite various diagnostic tools, depression in PwP may remain undiagnosed [3,4]. This study aims to ascertain the prevalence of the risk of depression without a formal diagnosis in PwP.
Method: Data analysis was conducted on the REMEPARKv2 protocol database, encompassing PwP recruited from July 2021 to February 2024. Key variables included prior depression diagnosis, Hamilton Depression Rating Scale (HDRS) scores (≥8 interpreted as risk of depression), and self-perceived depressive symptoms. Kappa concordance tests evaluated the utility of self-perception in diagnosing depression in PwP.
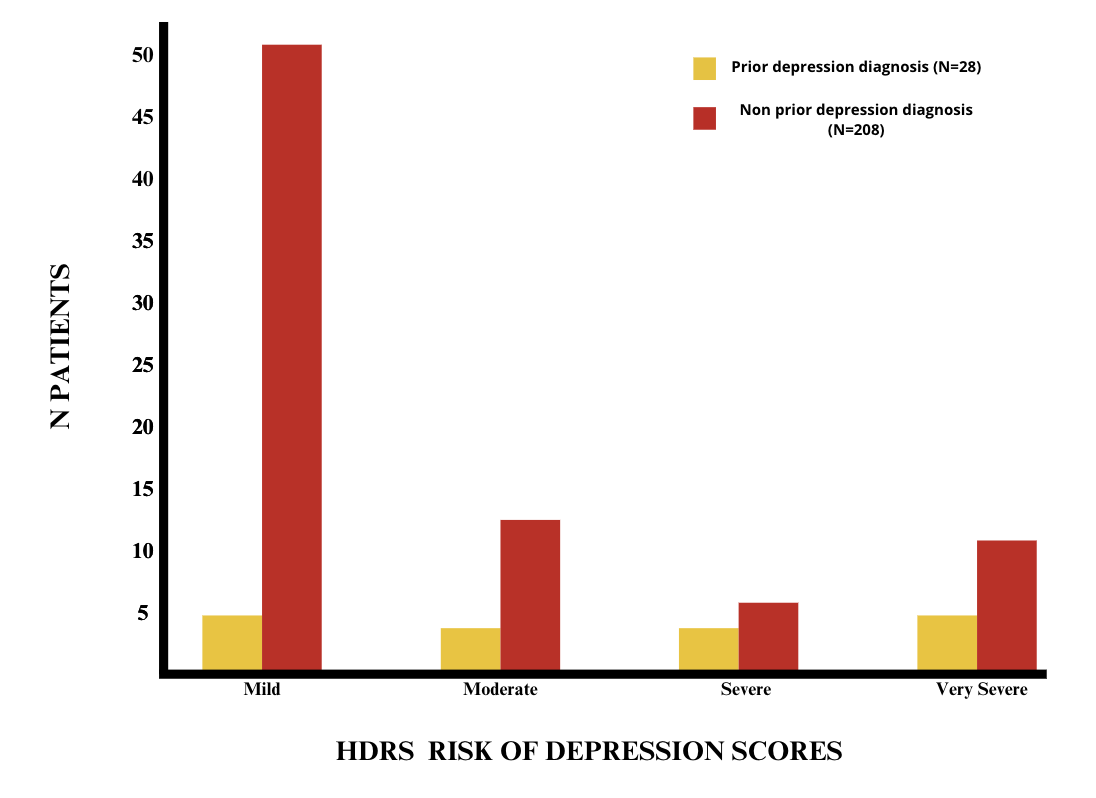
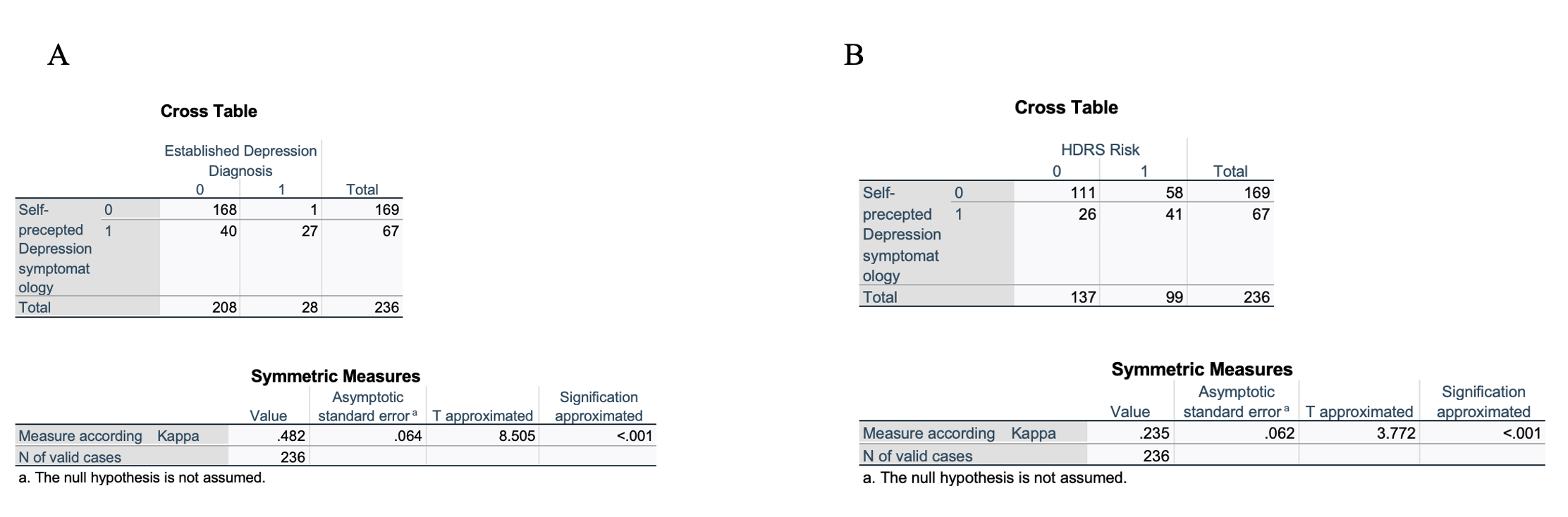
Results: Among 236 recruited patients (53% male, 47% female, mean age 65.19 ± 11.9 years, PD duration 7.5 ± 5.6 years). As detailed in Figure 1, 28 patients had a previous depression diagnosis. Of the 208 without prior diagnosis, 81 (38%) exhibited depression risk, comprising mild (63%), moderate (16%), severe (7%), and very severe (14%) categories. Kappa concordance tests revealed moderate agreement between self-reported depressive symptoms and diagnosed depression (K=0.482, p<0.001), and mild agreement between self-reported depressive symptoms and HDRS scores indicating depression risk (K=0.235, p<0.001) (Figure 2).
Conclusion: This analysis unveils a 36% prevalence of risk of undiagnosed depression among PwP. Notably, patients may experience severe depressive symptoms without formal diagnosis or management. Self-perceived depressive symptoms significantly correlate with diagnosed depression and HDRS scores, suggesting risk of depression. These findings emphasize the importance of deliberately addressing depressive symptoms in clinical practice, given the substantial portion of PwP at risk of undiagnosed depression, potentially impacting quality of life and disease progression. Limitations include sample size and reliance on a single depression assessment tool.
Figure 1
Figure 2
References: 1-Dallé E, Mabandla MV. Early Life Stress, Depression And Parkinson’s Disease: A New Approach. Mol Brain. 2018 Mar 19;11:18. doi: 10.1186/s13041-018-0356-9.
2-Cong S, Xiang C, Zhang S, Zhang T, Wang H, Cong S. Prevalence and clinical aspects of depression in Parkinson’s disease: A systematic review and meta‑analysis of 129 studies. Neurosci Biobehav Rev. 2022 Oct;141:104749. doi: 10.1016/j.neubiorev.2022.104749.
3-DeMarco EC, Al-Hammadi N, Hinyard L. Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis. Int J Environ Res Public Health. 2021 Aug 14;18:8596. doi: 10.3390/ijerph18168596.
4-Sujith P, Arjunan P, Iype T, Natarajan V. Depression in Patients With Parkinson’s Disease: A Hospital-Based Cross-Sectional Study. Cureus. 2023 Oct 17;15:e47214. doi: 10.7759/cureus.47214.
To cite this abstract in AMA style:
G. Rivera-Monroy, RJ. Baños-Betancourt, K. Velázquez-Román, CF. álvarez-Hernández, AL. Guerra-Anzaldo, WF. Moguel-Cardín, A. Domínguez-García, MF. Medina-Pérez, JC. Delgado-Uriarte, NP. Moreno-Aldama, A. Uribe-León, MC. Unda-Mcfarlane, AJ. Hernández-Medrano, A. Cervantes-Arriaga, M. Rodríguez-Violante. Listening to the Insight: The Underdiagnosis of Depression in People Living with Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/listening-to-the-insight-the-underdiagnosis-of-depression-in-people-living-with-parkinsons-disease/. Accessed March 29, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/listening-to-the-insight-the-underdiagnosis-of-depression-in-people-living-with-parkinsons-disease/