Category: Parkinson’s Disease: Clinical Trials
Objective: To evaluate and compare the trunk postural control of the elderly individuals with and without Parkinson’s disease (PD), using an unstable chair prototype.
Background: Effective trunk control is essential for good posture, postural stability and functional independence. In PD, muscle stiffness (rigidity), bradykinesia, postural instability, altered postural adjustment mechanisms and lack of trunk mobility have been associated with balance and functional mobility deficits, and risk of falling [1]-[3]. However, there is still a lack of specific and accurate instruments for assessing trunk postural control.
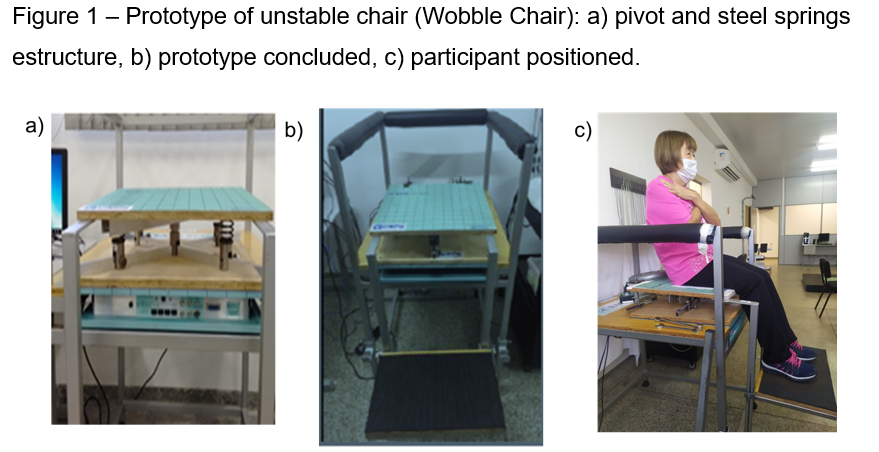
Method: Individuals with and without mild to moderate PD were assessed by the prototype of unstable chair Wobble Chair (Figure 1), in sitting upright position, feet supported to remain hips and knees in 90°, and looking at a target positioned 2.5m in front of them, at eye lines. We evaluated four conditions: 1) eyes open; 2) eyes closed; 3) dual task (i.e., Stroop test); and 4) no feet support. Each condition was performed twice for 30 seconds, with 30 seconds interval between them. For all conditions, were calculated center of pressure (COP) area (cm²), anteroposterior (AP) and mediolateral (ML) amplitudes (cm) and velocities (cm/s).
The comparison between conditions in both groups was performed using Friedman’s test. For intergroups comparison was used Mann Whitney test, according to data normality (p<0.05).
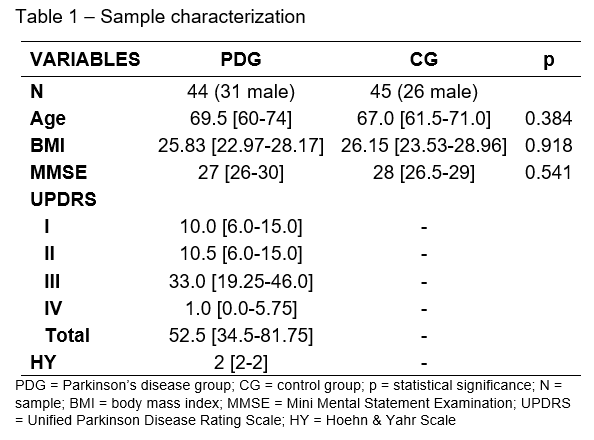
Results: Forty-four participants with PD and 45 healthy controls were assessed. There were no demographic differences between the groups at baseline (Table1).
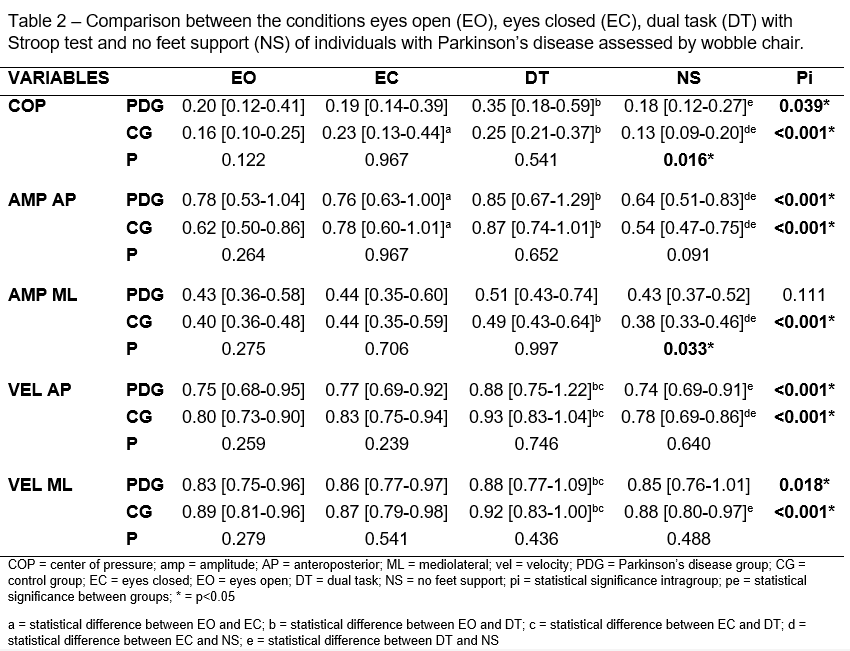
In intragroup analysis, results were similar for eyes open and no feet support conditions; and compared with those, eyes closed and dual-task conditions were harder to perform (higher oscillation), for both groups. Interestingly, dual task was more challenging then eyes closed condition (increased AP and ML velocity) for both groups. In intergroup analysis, individuals with PD had more difficulty with no feet support, with higher COP area (p=0.02) and ML amplitude (p=0.03) (Table 2).
Conclusion: The suppression of visual input or addition of dual task increased the difficulty of maintaining trunk postural control for individuals with and without PD. Moreover, individuals with PD showed additional difficulty when the feet support was removed, as more active trunk control is required.
References: [1] S. Cao, Y. Cui, J. Jin, F. Li, X. Liu, and T. Feng, “Prevalence of axial postural abnormalities and their subtypes in Parkinson’s disease: a systematic review and meta-analysis,” J. Neurol., 2022, doi: 10.1007/s00415-022-11354-x.
[2] R. P. Hubble, P. A. Silburn, G. A. Naughton, and M. H. Cole, “Trunk exercises improve balance in Parkinson disease: A phase II randomized controlled trial,” J. Neurol. Phys. Ther., vol. 43, no. 2, pp. 96–105, 2019, doi: 10.1097/NPT.0000000000000258.
[3] N. Ö. Ünlüer, T. Ozkan, Y. A. Sari, and Y. S. Karadağ, “Investigation of the relationship between trunk position sense and balance, functional mobility, fear of falling, and disease stage in Parkinson’s disease,” Ir. J. Med. Sci., 2022, doi: 10.1007/s11845-022-03192-7.
To cite this abstract in AMA style:
H A. Araújo, A. Melanda, R. da Silva, S. Smaili. Is there impairment in neuromuscular trunk control in Parkinson disease when compared to healthy elderly? [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/is-there-impairment-in-neuromuscular-trunk-control-in-parkinson-disease-when-compared-to-healthy-elderly/. Accessed December 6, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/is-there-impairment-in-neuromuscular-trunk-control-in-parkinson-disease-when-compared-to-healthy-elderly/