Session Information
Date: Wednesday, September 25, 2019
Session Title: Cognition and Cognitive Disorders
Session Time: 1:15pm-2:45pm
Location: Agora 3 East, Level 3
Objective: To assess whether diagnostic rates of both Parkinson’s disease dementia (PDD) and dementia with Lewy bodies (DLB) could be increased by the introduction of a structured assessment toolkit for clinicians.
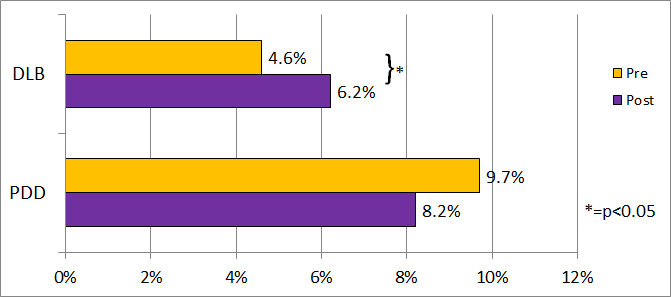
Background: Diagnostic rates for DLB and PDD in clinical practice in the UK were recently found to be 4.6% and 9.7% respectively [1]. The rate of DLB was below that found in pathological studies, which report a rate of more than 15%. The proportion of Parkinson’s disease (PD) cases with dementia was also below that expected, with the majority of clinical studies revealing a prevalence of between 20% and 30%.
Method: An assessment toolkit was produced based on the established diagnostic criteria for DLB and PDD, with the aim of providing a structured framework for clinicians to assess patients suspected of either condition [2][3]. The toolkits were introduced to clinicians working in services within the North East and East Anglia within the UK, the same two regions we previously sampled. Teaching sessions on using the toolkits were provided to clinicians by the investigators. In total, four memory clinics and three movement disorder/PD clinics were then reassessed for the rate of diagnosis of DLB and PDD, respectively, using exactly the same methodology previously used to ascertain baseline diagnostic rates.
Results: For DLB, 2058 case notes were reviewed from memory clinics and DLB was diagnosed in 6.2% of dementia cases [figure 1]. This is an absolute rise of 1.6%, equal to a 35% increase in the cases diagnosed, compared to the previously reported rate of 4.6% prior to the introduction of the DLB toolkit (P=0.021). With respect to PDD, 3405 case notes were reviewed from movement disorder or PD clinics across the two regions. The number of PD patients diagnosed with PDD was not found overall to be significantly different after the introduction of the toolkit: 8.2% compared to the prior rate of 9.7%, P=0.09, though with some variation between regions.
Conclusion: Introduction of the assessment toolkit significantly increased the rate of DLB diagnosis, suggesting that a structured means of assessing patients for DLB could assist clinicians and improve rates of diagnosis. The assessment toolkit did not alter the overall rate of PDD diagnosis, meaning alternate means may be required to improve the rate of diagnosis of dementia in Parkinson’s disease.
References: [1] Kane, J.P.M. et al., 2018. Clinical prevalence of Lewy body dementia. Alzheimer’s research & therapy, 10(1), p.19. [2] Thomas, A.J. et al., 2017. Development of assessment toolkits for improving the diagnosis of the Lewy body dementias: feasibility study within the DIAMOND Lewy study. International Journal of Geriatric Psychiatry, 32(12), pp.1280–1304. [3] Thomas, A.J. et al., 2018. Revision of assessment toolkits for improving the diagnosis of Lewy body dementia: The DIAMOND Lewy study. International Journal of Geriatric Psychiatry, (January), pp.1293–1304..
To cite this abstract in AMA style:
A. Surendranathan, J. Kane, A. Bentley, S. Barker, J. Taylor, A. Thomas, I. Mckeith, D. Burn, J. O'Brien. Introduction of an Assessment Toolkit Increases the Rate of DLB Diagnosis [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/introduction-of-an-assessment-toolkit-increases-the-rate-of-dlb-diagnosis/. Accessed December 25, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/introduction-of-an-assessment-toolkit-increases-the-rate-of-dlb-diagnosis/