Category: Education in Movement Disorders
Objective: To implement a neuropalliative care curriculum for neurology residents in order to increase comfort with palliative and hospice care topics for patients with progressive neurodegenerative diseases.
Background: Currently, few neurology programs have a formalized palliative care curriculum even though instruction in palliative care is an ACGME requirement for residency training programs. Many publications show the importance of palliative care in neurology. The majority of informal instruction on the topic during training occurs with acute neurologic changes or during ICU hospitalizations. More consistent instruction focused on outpatient palliative care discussions of those with chronic neurodegenerative disease is needed.
Method: A 3 hour curriculum was implemented in 2019 and led by a palliative care specialist.
Pre- and post-surveys curriculum surveys were administered.
Inclusion Criteria: All neurology residents who agreed to participate.
Exclusion Criteria: Non-residents (including fellows, medical students, APPs).
Statistical analysis: Unpaired t-test analyses were performed to determine if any of the responses demonstrated a statistically significant change after the curriculum was implemented, with a statistical significance defined as p < 0.05.
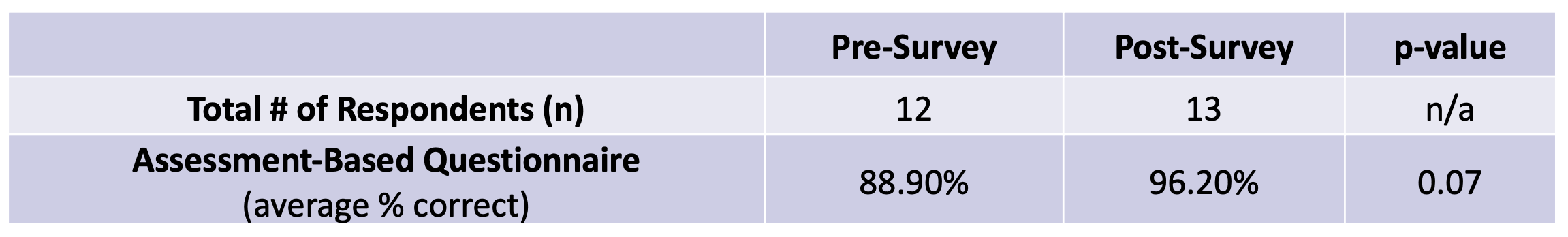
Results: [Figure 1]
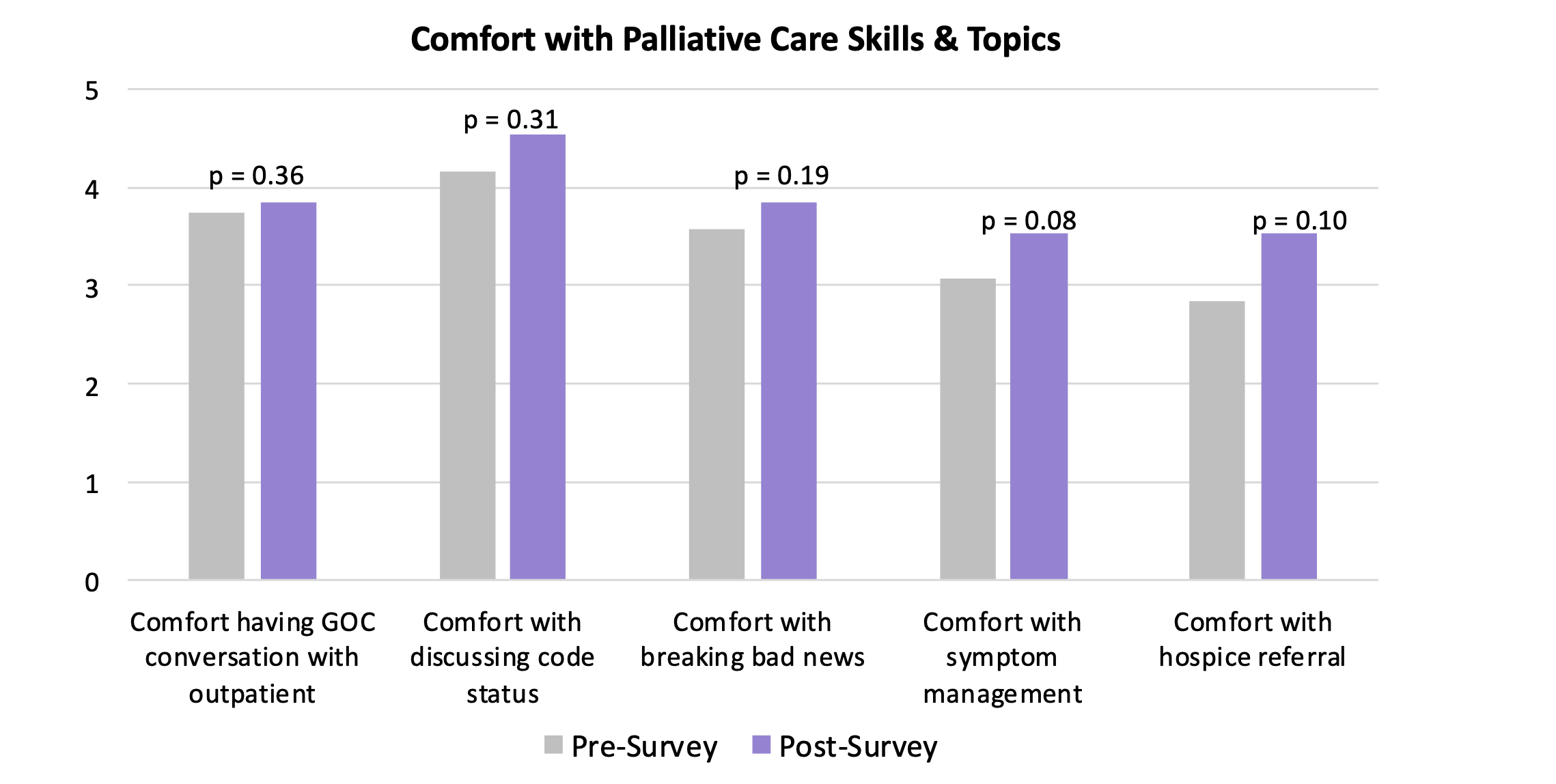
[Figure 2]
There were approximately 20 learners at each session. On the knowledge-based questions, the average score improved from 89% to 96%. After the completion of the curriculum, residents said they felt more comfortable having goals of care discussions with a patient with a chronic neurodegenerative disease, discussing code status, breaking bad news, managing symptoms, and referring to hospice. All 12 residents who filled out the pre-survey either agreed (n=3) or strongly agreed (n=9) that structured education in palliative care was needed. After the curriculum, 12 residents who filled out the post-survey either agreed (n=3) or strongly agreed (n=9) that the curriculum was valuable, 1 resident disagreed. All 13 residents who filled out the post-survey stated they would apply what they learned to their practice.
Conclusion: A three hour neuropalliative care curriculum for neurology residents led by a palliative care specialist resulted in improved comfort level with palliative care topics and skills related to patients with chronic neurodegenerative disorders.
References: 1. ACGME Program Requirements for Graduate Medical Education in Neurology. Available at: http://www.acgme.org. Accessed May, 2019. 2. I. Boersma, J. Miyasaki, J. Kutner, B. Kluger, Palliative care and neurology: Time for a paradigm shift. Neurology. 83, 561–567 (2014). 3. D. Kern, P. Thomas, M. Hughes, in Curriculum Development for Medical Education (Johns Hopkins University Press, Baltimore, ed. 2nd, 2009), pp. 6–42. 4. A. K. Mehta, S. Najjar, N. May, B. Shah, L. Blackhall, A Needs Assessment of Palliative Care Education among the United States Adult Neurology Residency Programs. Journal of Palliative Medicine. 21, 1448–1457 (2018). 5. N. Karlen, B. Cruz, A. E. Leigh, Resident-Led Palliative Care Education Project. Journal of Palliative Medicine. 19, 428–436 (2016).
To cite this abstract in AMA style:
O. Dubaz, J. Hauser. Implementing a Neuropalliative Care Curriculum for Neurology Residents Focused on Neurodegenerative Diseases [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/implementing-a-neuropalliative-care-curriculum-for-neurology-residents-focused-on-neurodegenerative-diseases/. Accessed January 7, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/implementing-a-neuropalliative-care-curriculum-for-neurology-residents-focused-on-neurodegenerative-diseases/