Category: Epidemiology
Objective: To evaluate the impact of the COVID-19 pandemic on accessibility to deep brain stimulation (DBS) care at a tertiary DBS center
Background: Early responses to the COVID-19 pandemic utilized intermittent lockdowns and social distancing. In the United States, this resulted in periodic suspension of elective surgeries. At the University of Florida (UF), we experienced several periods where DBS lead implantation surgeries were postponed or delayed. This study aimed to characterize and evaluate the impact of delayed surgical care and its impact on patient outcomes
Method: We conducted a retrospective study of all patients who underwent DBS lead implantation at UF from January 2019 to December 2021. Demographic data including preoperative evaluation visit and post operative DBS visits were collected. These dates were used to calculate the time from DBS interdisciplinary pre-surgical evaluation and pre-operative clinical evaluation per the Unified Parkinson’s disease rating scale (UPDRS) to the date of DBS lead implantation. Patients were categorized by the year of DBS implantation (i.e., 2019, 2020 and 2021). Data homoscedasticity was evaluated using Bartlett’s test. Group-wise comparisons were conducted using the non-parametric Kruskal-Wallis test.
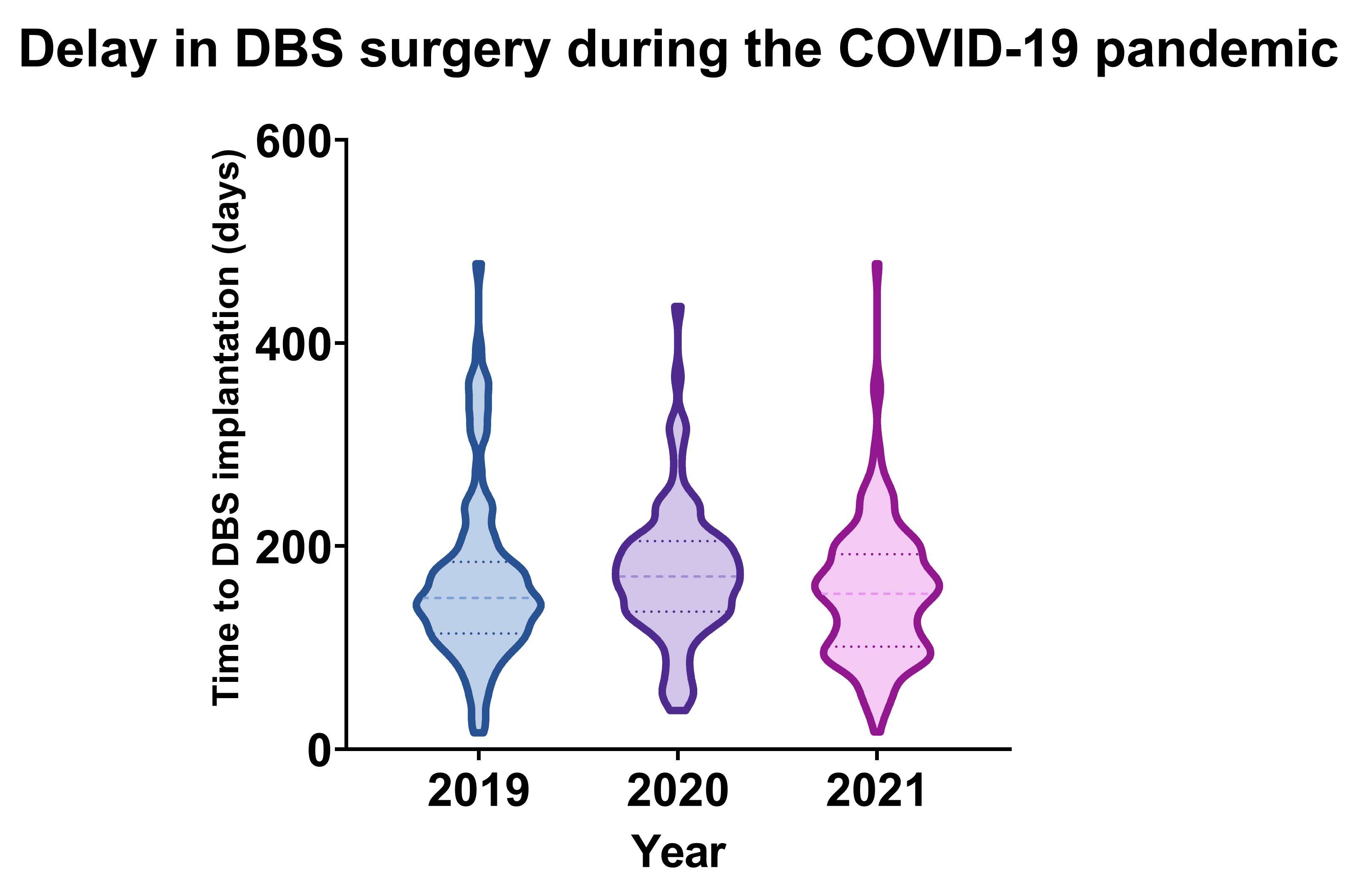
Results: 387 patients were identified and analyzed in this study. The data set failed Bartlett’s test of homoscedasticity, therefore the Kruskal-Wallis test was used to compare the mean time differences across the 3 years. There was a significant difference in mean time from DBS interdisciplinary pre-surgical evaluation to the date of DBS lead implantation (p = 0.0319). The mean (SD) time from pre-surgical assessment to DBS implantation (figure 1) were: 166.37 (83.27) days in 2019, 173.45 (66.34) days in 2020, and 153.20 (65.99) days in 2021. The time from pre-operative UPDRS to DBS implantation trended towards but did not reach significance (p=0.3868). The mean (SD) time from pre-operative UPDRS evaluation to DBS implantation was: 196.56 (88.19) days in 2019, 234.91 (124.71) days in 2020, and 231.44 (134.72) days in 2021
Conclusion: The COVID-19 pandemic prolonged both time to surgery and time since pre-operative clinical evaluation. Although unavoidable, these types of delay can affect the perception of post-operative outcomes through disease progression. These factors should be taken into account during DBS studies conducted during the pandemic era.
References: [1] Shao, Connie C., M. Chandler McLeod, Lauren Gleason, Isabel C. Dos Santos Marques, Daniel I. Chu, and Drew Gunnells. 2022. “Effect of COVID-19 Pandemic Restructuring on Surgical Volume and Outcomes of Non-COVID Patients Undergoing Surgery.” The American Surgeon 88 (3): 489–97.
To cite this abstract in AMA style:
F. Sarmento, S. Aghili-Mehrizi, T. de Araujo, J. Wong. Impact of the COVID-19 pandemic on DBS accessibility: a single center experience [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/impact-of-the-covid-19-pandemic-on-dbs-accessibility-a-single-center-experience/. Accessed January 17, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/impact-of-the-covid-19-pandemic-on-dbs-accessibility-a-single-center-experience/