Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To investigate the sleep problems and circadian rhythm abnormalities in PD patients using sleep evaluation scale – Parkinsons disease sleep scale (PDSS) for mild sleep disturbances, Munich’s chrono type questionnaire and morning-ness and evening-ness questionnaire.
To measure the serum levels of melatonin during night-sleep in PD patients and to identify any association with sleep problems or chronotype.
Background: Sleep disturbances are common and can significantly worsen the motor problems of PD. Sleep can vary in timing based on chronotype ( ‘lark’ or ‘owl’), which is genetically manifested. Currently there are no studies on how chronotype along with melatonin levels can influence sleep disturbances in PD patients.
Method: A prospective cross-sectional study from December 2018 to November 2019 was conducted with a total of 100 patients with PD. Clinical and demographic data were analysed, sleep disorders and circadian rhythm abnormalities measured using morningness eveningness questionnaire, Munich’s chrono type questionnaire, Parkinson disease sleep scales. Serum melatonin levels in 50 patients and 30 controls at 12 am and 5 am were assessed using ELISA kits.
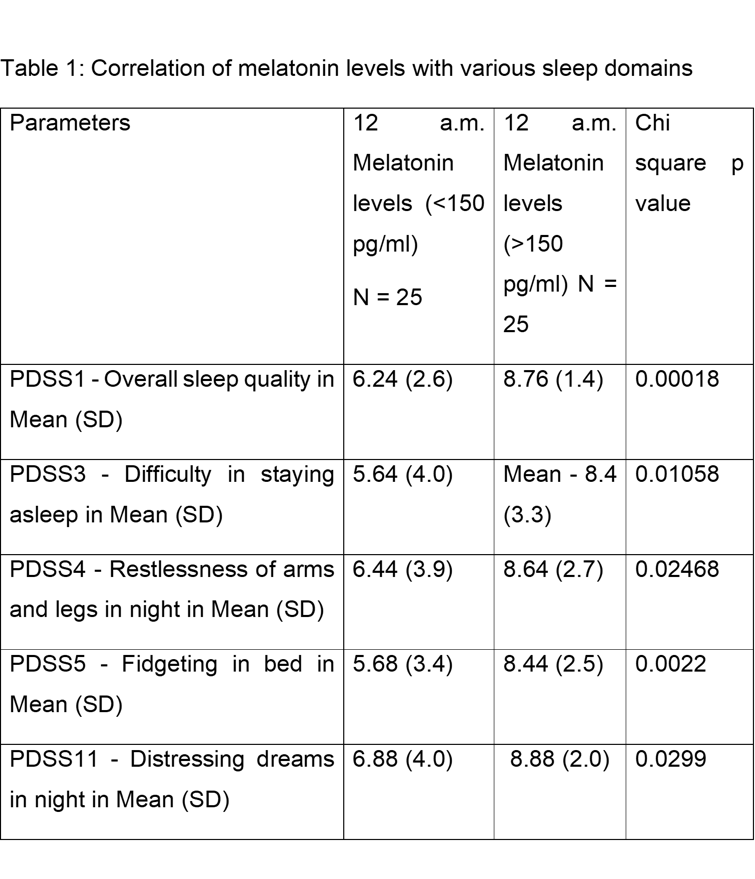
Results: Mean age was 56.14±10 years, mean age of onset 49.4± 11 years, mean duration of disease was 6.76+0.4 years. 86% of patients had sleep onset before 11PM. 46% were moderately morning type while 42% were definitely morning type. Mean Total PDSS score was 114 +30. Only 5 patients had a normal score. Most common sleep disturbances were getting up at night to pass urine(mean 5.45± 3.9) and experiencing tremor on waking up( mean 6.4±4) and least reported was painful posturing of limbs causing early morning awakenings(mean 8.9±2.6). Mean melatonin levels in patients were significantly lower than controls at 12 a.m. and 5 a.m. On further dichotimising the population based on melatonin levels at 12 am, we found statistically significant correlation of lower melatonin levels with higher UPDRS 1, poorer overall quality of sleep,few sleep domains (table 1) and no significant correlation with age of the patient, duration or severity of disease and chronotype.
Conclusion: Sleep disturbances were common among PD patients. Most of PD patients were morning chronotype. Serum melatonin levels were lower among the PD population compared to controls. Serum melatonin but not the chronotype was associated with poorer quality of sleep.
To cite this abstract in AMA style:
R. Borgohain, M. Voodi, R. Kandadai, S. Meka, T. Syed, S. Turaga. Impact of Chronotypes and melatonin levels on sleep disorders in patients with Parkinson’s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/impact-of-chronotypes-and-melatonin-levels-on-sleep-disorders-in-patients-with-parkinsons-disease/. Accessed April 26, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/impact-of-chronotypes-and-melatonin-levels-on-sleep-disorders-in-patients-with-parkinsons-disease/