Category: Surgical Therapy: Parkinson's Disease
Objective: Evaluate whether if electrodes reconstruction using Lead-DBS, an open source toolbox, in patients with Parkinson’s Disease (PwPDP) treated with Deep Brain Stimulation (DBS) presenting with Stimulation-Related Side Effects (SRSE) could help with the troubleshooting workflow.
Background: Electrodes position is an essential part of successful DBS treatment. By analyzing their exact localization inside the target and their relationship with neighboring structures, we can predict the beneficial stimulation effects and possible SRSE.
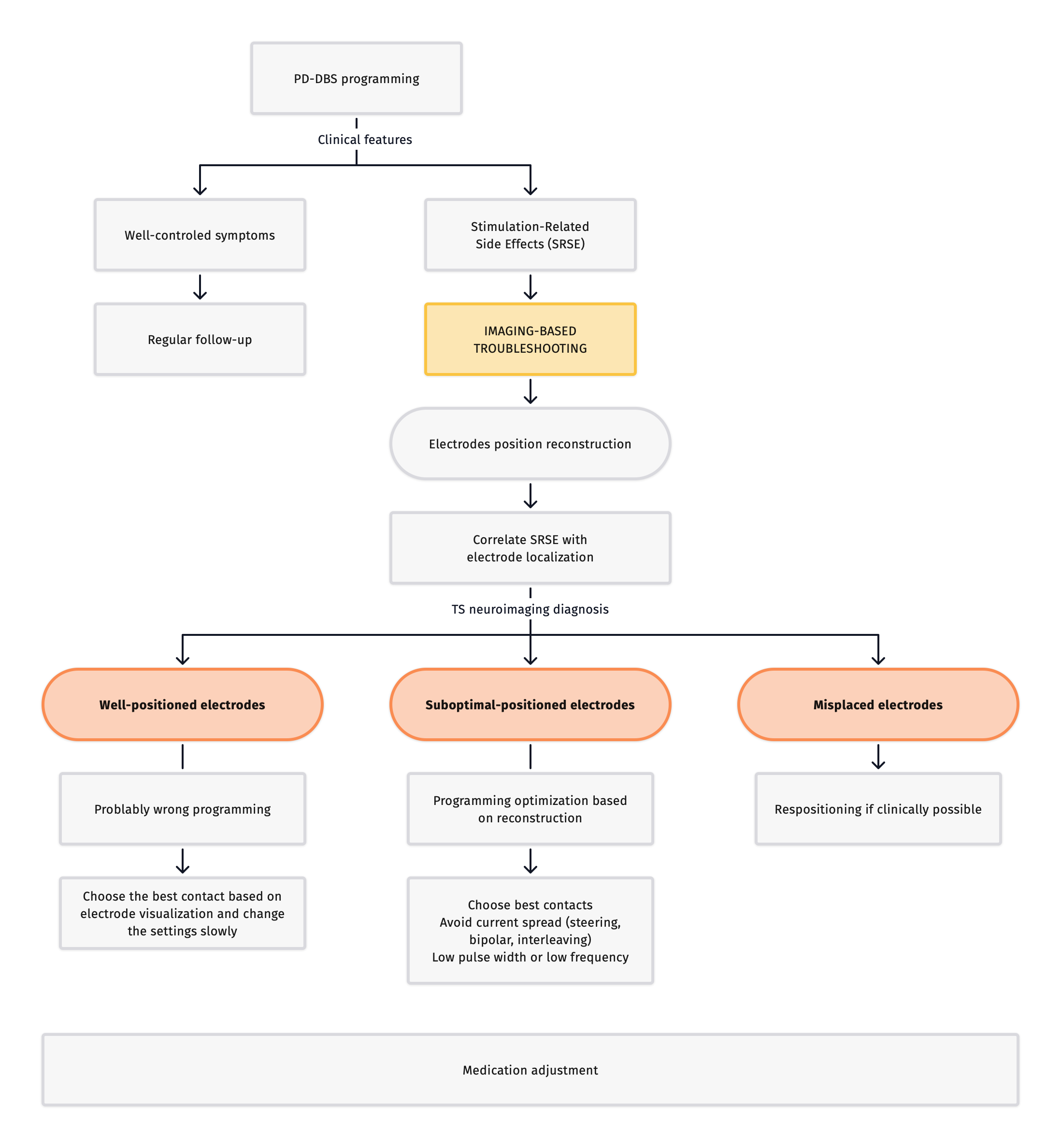
Method: The inclusion criteria were PwPD treated with DBS with any SRSE that limited therapy optimization from the Neuromodulation Clinic of the University of São Paulo (USP) between 2021-2023. The electrodes of the selected patients were reconstructed with the open-source toolbox LeadDBS using preoperative MRI and postoperative CT. After the reconstruction, the electrode position within the target was classified in (1) well-positioned; (2) suboptimal-positioned; and (3) misplaced. Then, if there was positive a clinical-imaging correlation, solutions were suggested to minimize side effects based on the Volume of the Tissue Activated (VTA) visualization.
Results:
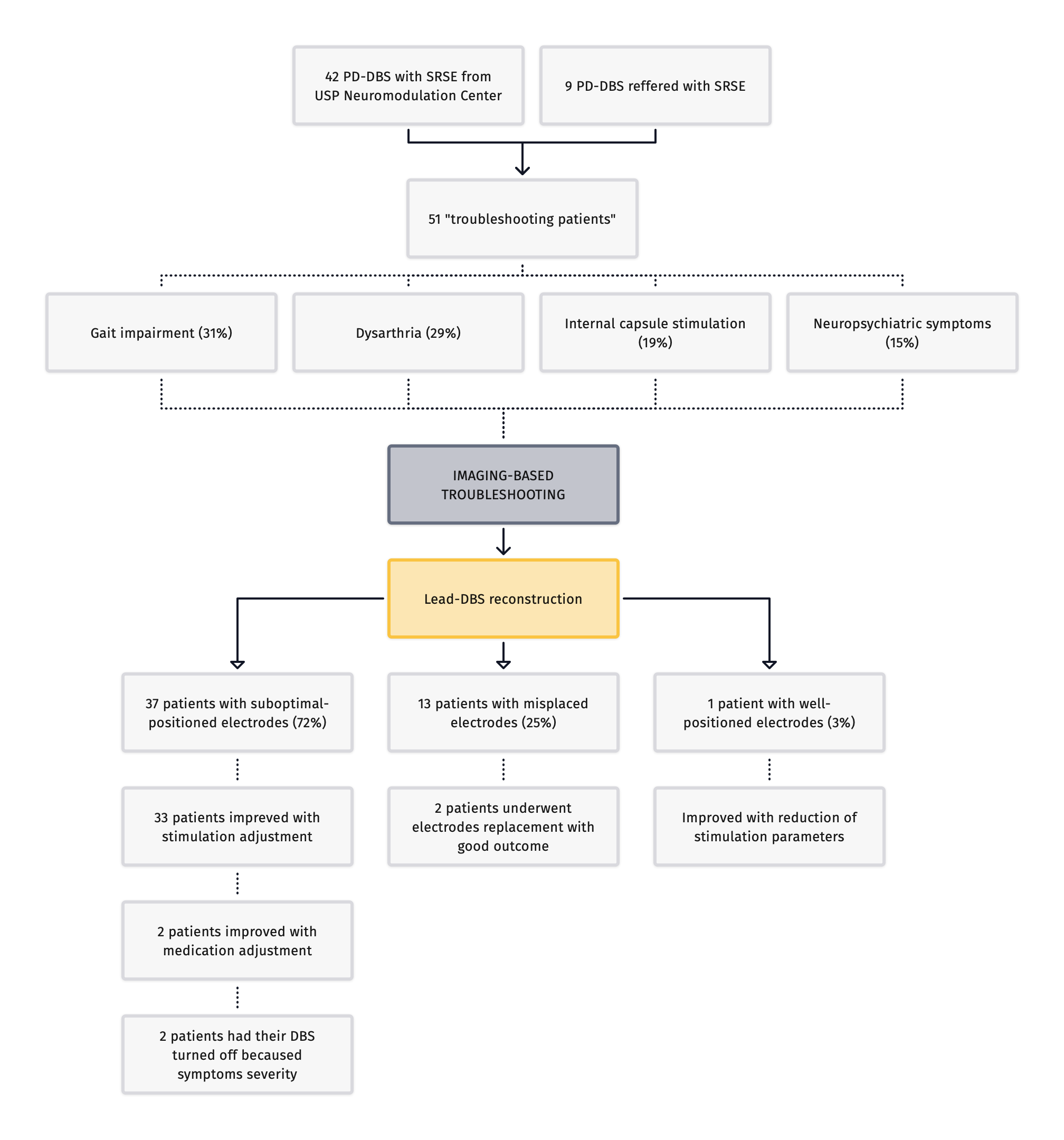
A total of 51 patients were included. SRSE reported were gait impairment (31%), dysarthria (29%), internal capsule stimulation-related symptoms (21%), and neuropsychiatric issues (15%).Electrodes reconstruction showed: 72% had at least one suboptimal-positioned electrode, 25% had at least one misplaced electrode, and only 3% had well-positioned electrodes. 97% of patients had a positive clinical-imaging correlation. Two patients in the misplaced group underwent the repositioning procedure with improvement. Two patients of suboptimal-positioned group had the DBS therapy turned off because of neuropsychiatric symptoms. Two suboptimal-positioned group patients improved with medication adjustment. The others thirty-three with suboptimal-position positions had improved SRSE using steering, bipolar, interleaving, low-frequency, low-pulse-width, and cycling strategies. The patient with well-positioned electrode improved after parameters change. Figure 1 shows the results.
Conclusion:
Troubleshooting after DBS in PD are common and electrodes reconstruction can help the clinician with the diagnosis workflow and management (Figure 2) by correlating the reconstruction findings with the patient´s symptoms.
Figure 1 – Results fluxogram
Figure 2 – Imaging guided troubleshooting
References: 1. Castrioto A, Lozano AM, Poon YY, Lang AE, Fallis M, Moro E. Ten-year outcome of subthalamic stimulation in Parkinson disease: a blinded evaluation. Arch Neurol. 2011;68(12):1550-1556. doi:10.1001/archneurol.2011.182
2. Neudorfer C, Butenko K, Oxenford S, et al. Lead-DBS v3.0: Mapping deep brain stimulation effects to local anatomy and global networks. Neuroimage. 2023;268:119862. doi:10.1016/j.neuroimage.2023.119862
3. Vilkhu G, Goas C, Miller JA, et al. Clinician vs. imaging-based subthalamic nucleus deep brain stimulation programming. Parkinsonism Relat Disord. 2023;106:105241. doi:10.1016/j.parkreldis.2022.105241
4. Lange F, Steigerwald F, Malzacher T, et al. Reduced Programming Time and Strong Symptom Control Even in Chronic Course Through Imaging-Based DBS Programming. Front Neurol. 2021;12:785529. doi:10.3389/fneur.2021.785529
5. Farris S, Giroux M. Retrospective review of factors leading to dissatisfaction with subthalamic nucleus deep brain stimulation during long-term management. Surg Neurol Int. 2013;4:69. doi:10.4103/2152-7806.112612
To cite this abstract in AMA style:
J. Yamamoto, I. Paraguay, R. Barbosa, E. Barbosa, R. Cury. Imaging-based Troubleshooting Deep Brain Stimulation in Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/imaging-based-troubleshooting-deep-brain-stimulation-in-parkinsons-disease/. Accessed December 16, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/imaging-based-troubleshooting-deep-brain-stimulation-in-parkinsons-disease/