Category: Parkinsonism, Atypical: PSP, CBD
Objective: We describe a case of NPH-like presentation of PSP, review literature surrounding this entity, and discuss key diagnostic considerations and implications.
Background: Despite advances in neuroimaging and neuropsychological testing, diagnosing progressive supranuclear palsy (PSP) and normal pressure hydrocephalus (NPH) remains challenging due to overlapping clinical presentations and neuroimaging findings, especially in early stages.
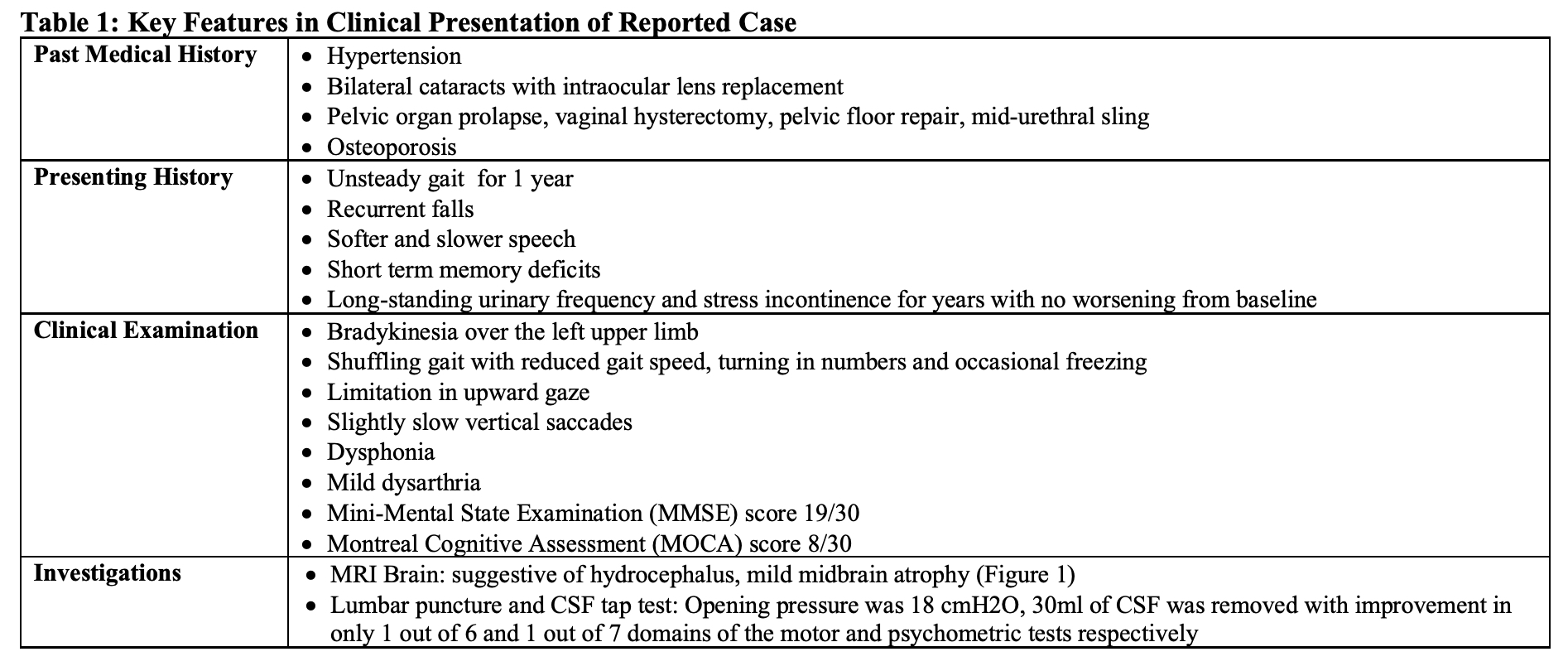
Method: We assessed a 76-year-old lady who presented with gait disturbance and cognitive impairment. Table 1 details her clinical presentation.
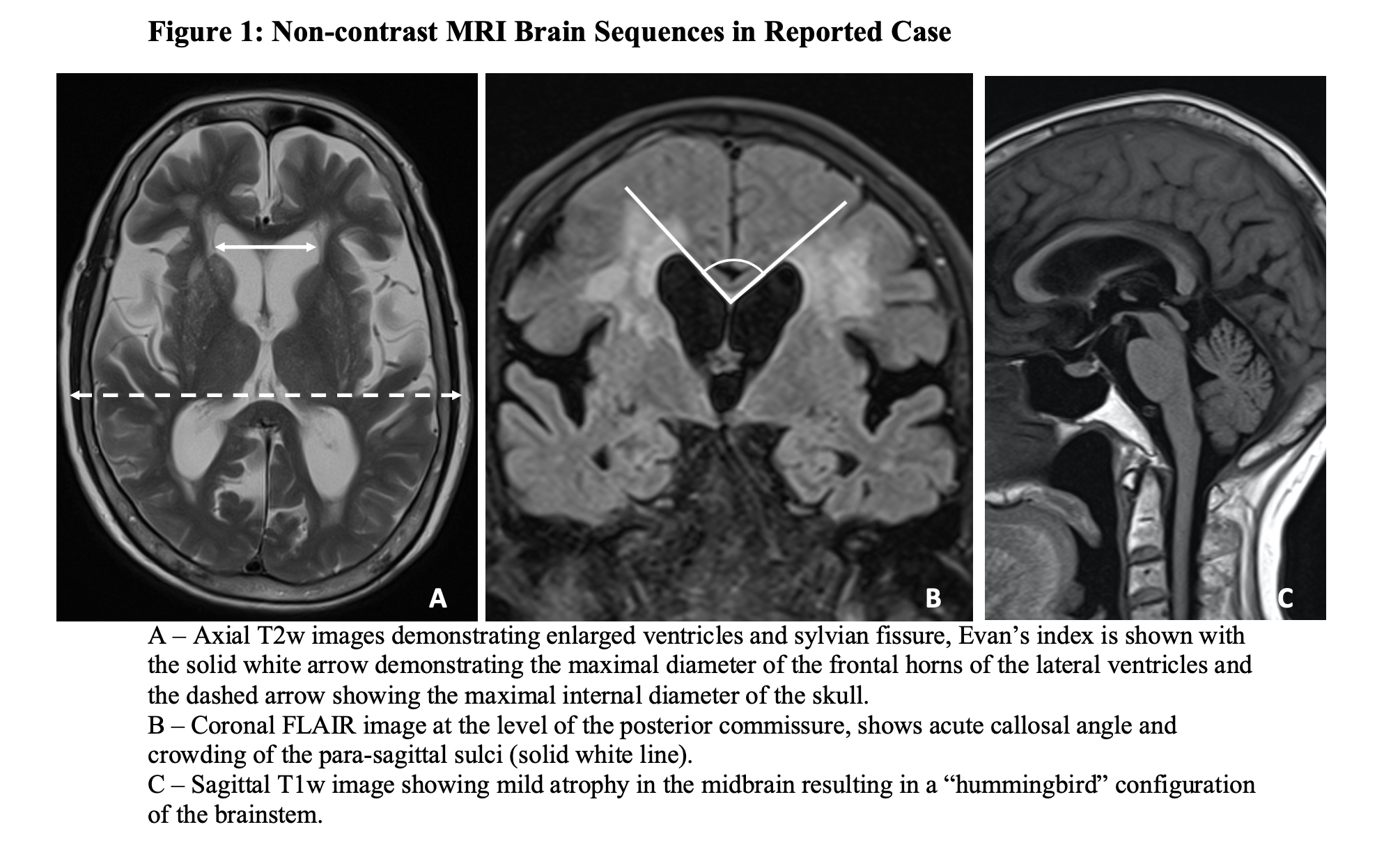
Results: Laboratory tests were unremarkable. MRI Brain suggested NPH (Figure 1). The MRI findings were reviewed with the hospital’s radiologist, who opined that the imaging features favoured NPH over PSP. Subsequent cerebrospinal fluid (CSF) tap test was inconclusive (Table 1). The patient was counselled on the likelihood of PSP with a possibility of NPH involvement. The patient declined a repeat CSF tap test with more volume of CSF being drawn out. She was counselled on the likelihood of PSP with a possibility of NPH involvement, and was initiated on Levodopa/Benserazide with outpatient follow-up planned.
Conclusion: This case underscores the diagnostic challenge between PSP and NPH. While clinical findings were more suggestive of PSP, there was also hydrocephalus present on the MRI Brain which suggested NPH.
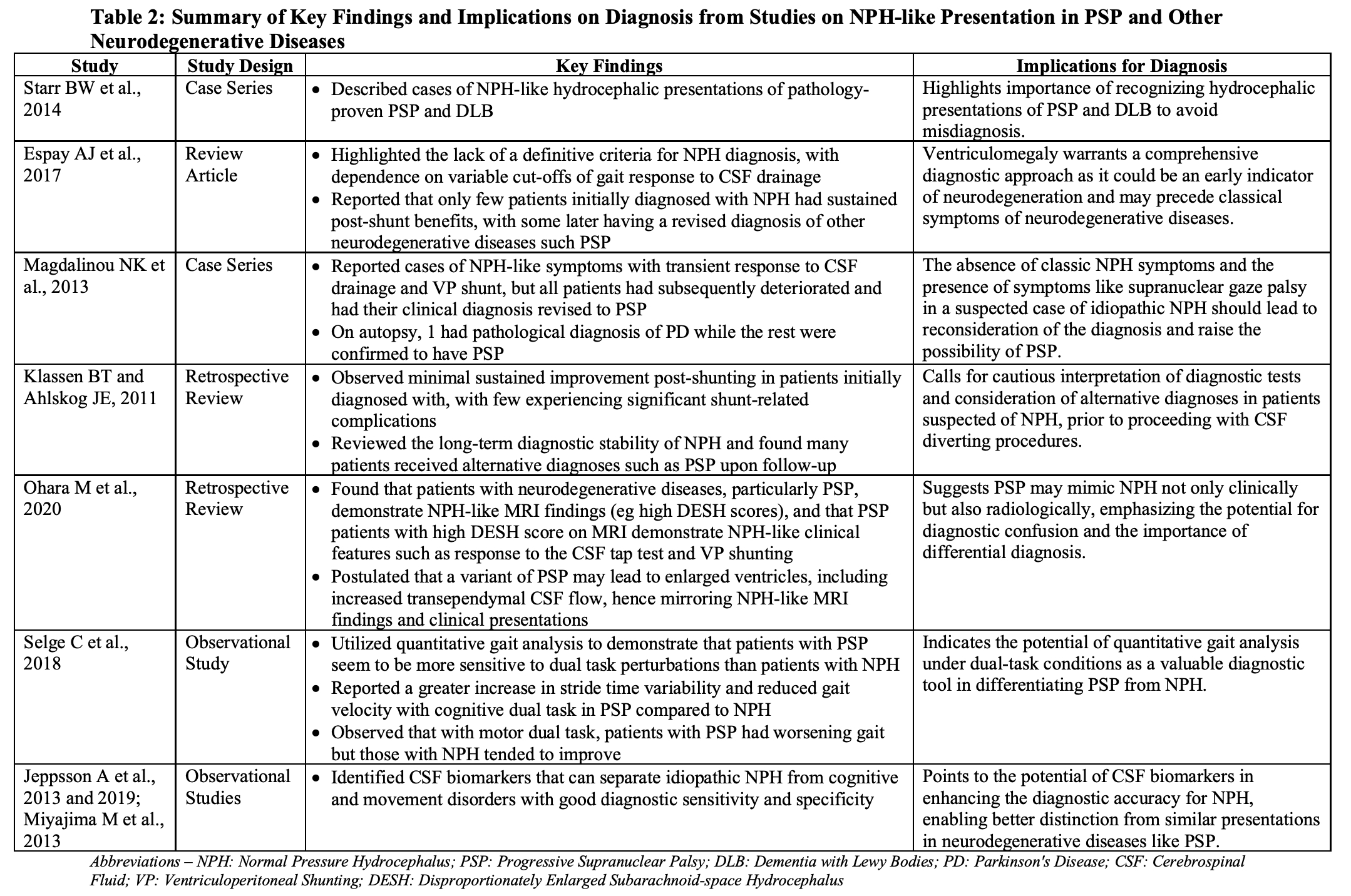
Prior studies[1-5], summarized in Table 2, have consistently shown that NPH-like hydrocephalus can be present in other neurodegenerative diseases, particularly in PSP. Thus, radiological hydrocephalus should be clinically contextualized. While it was reasonable to offer this patient a repeat CSF tap test, even if it were positive, it would not solely dictate the diagnosis of NPH and should still be interpreted in accordance with the overall clinical picture.
Our literature review also points to additional diagnostic tools[6-9], such as quantitative gait analysis and biomarkers, to differentiate NPH from PSP and other neurodegenerative diseases (Table 2). These have important implications on disease pathophysiology and a more definite diagnosis of NPH in the future.
NPH-like hydrocephalus can occur in other neurodegenerative diseases, emphasizing the need for clinical context in interpretation. Recognizing this “hydrocephalic presentation” can prevent unnecessary procedures and guide appropriate management.
Table 1
Figure 1
Table 2
References: [1] Starr BW, Hagen MC, Espay AJ. Hydrocephalic Parkinsonism: lessons from normal pressure hydrocephalus mimics. Journal of Clinical Movement Disorders 2014;1. https://doi.org/10.1186/2054-7072-1-2.
[2] Espay AJ, da Prat GA, Dwivedi AK, Rodriguez-Porcel F, Vaughan JE, Rosso M, et al. Deconstructing normal pressure hydrocephalus: Ventriculomegaly as early sign of neurodegeneration. Annals of Neurology 2017;82. https://doi.org/10.1002/ana.25046.
[3] Magdalinou NK, Ling H, Smith JDS, Schott JM, Watkins LD, Lees AJ. Normal pressure hydrocephalus or progressive supranuclear palsy? A clinicopathological case series. Journal of Neurology 2013;260. https://doi.org/10.1007/s00415-012-6745-6.
[4] Klassen BT, Ahlskog JE. Normal pressure hydrocephalus: How often does the diagnosis hold water? Neurology 2011;77. https://doi.org/10.1212/WNL.0b013e31822f02f5.
[5] Ohara M, Hattori T, Yokota T. Progressive supranuclear palsy often develops idiopathic normal pressure hydrocephalus-like magnetic resonance imaging features. European Journal of Neurology 2020;27. https://doi.org/10.1111/ene.14322.
[6] Selge C, Schoeberl F, Zwergal A, Nuebling G, Brandt T, Dieterich M, et al. Gait analysis in PSP and NPH. Neurology 2018;90. https://doi.org/10.1212/WNL.0000000000005168https://doi.org/10.1016/j.jalz.2010.12.008.
[7] Jeppsson A, Zetterberg H, Blennow K, Wikkelsø C. Idiopathic normal-pressure hydrocephalus Pathophysiology and diagnosis by
[8] Jeppsson A, Wikkelsö C, Blennow K, Zetterberg H, Constantinescu R, Remes AM, et al. CSF biomarkers distinguish idiopathic normal pressure hydrocephalus from its mimics. Journal of Neurology, Neurosurgery and Psychiatry 2019. https://doi.org/10.1136/jnnp-2019-320826.
[9] Miyajima M, Nakajima M, Ogino I, Miyata H, Motoi Y, Arai H. Soluble amyloid precursor protein α in the cerebrospinal fluid as a diagnostic and prognostic biomarker for idiopathic normal pressure hydrocephalus. European Journal of Neurology 2013;20. https://doi.org/10.1111/j.1468-1331.2012.03781.x.
To cite this abstract in AMA style:
A. Premkumar, D. Lim, SK. Seetharaman, LF. Tan. Hydrocephalic Progressive Supranuclear Palsy: An Underrecognized Entity [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/hydrocephalic-progressive-supranuclear-palsy-an-underrecognized-entity/. Accessed December 16, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/hydrocephalic-progressive-supranuclear-palsy-an-underrecognized-entity/