Category: Parkinson's Disease: Non-Motor Symptoms
Objective: The aim of the study was to investigate the possible correlation between non-motor symptoms (NMS) burden and quality of life (QoL) with hearing impairment (HI) in a large cohort of Parkinson’s disease (PD) patients, by means of pure tone audiometry (PTA) and distortion product otoacoustic emissions (DPOAEs).
Background: Sensorial NMS, which include pain, olfactory disturbance, visual and hearing impairment (HI), are often underestimated and untreated in clinical practice. Focusing on the auditory system, literature showed supported evidence of HI in PD [1] [2] , although it has rarely been correlated with other NMS.
Method: We selected patients with idiopathic PD, without other concomitant neurological diseases, dementia or diagnosis of any audiological/vestibular disease. Demographic and clinical data were collected (UPDRS III, disease duration, H&Y). Then, patients underwent otoscopic examination, audiological testing (PTA and DPOAEs) and questionnaires with NMSS and PDQ39. ANCOVA and partial correlation analysis with Pearson coefficient have been used for statistical analysis (p value<0,05).
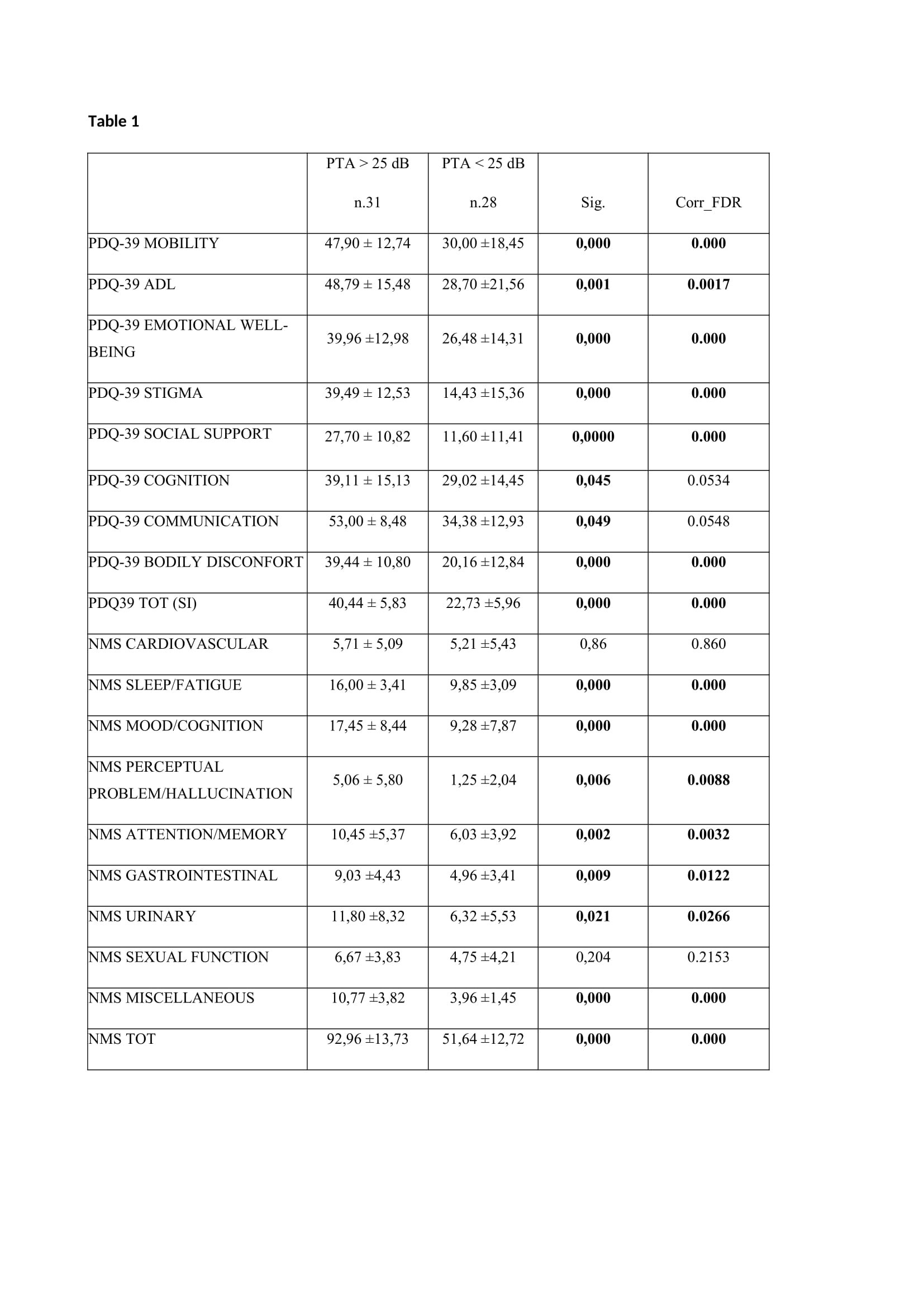
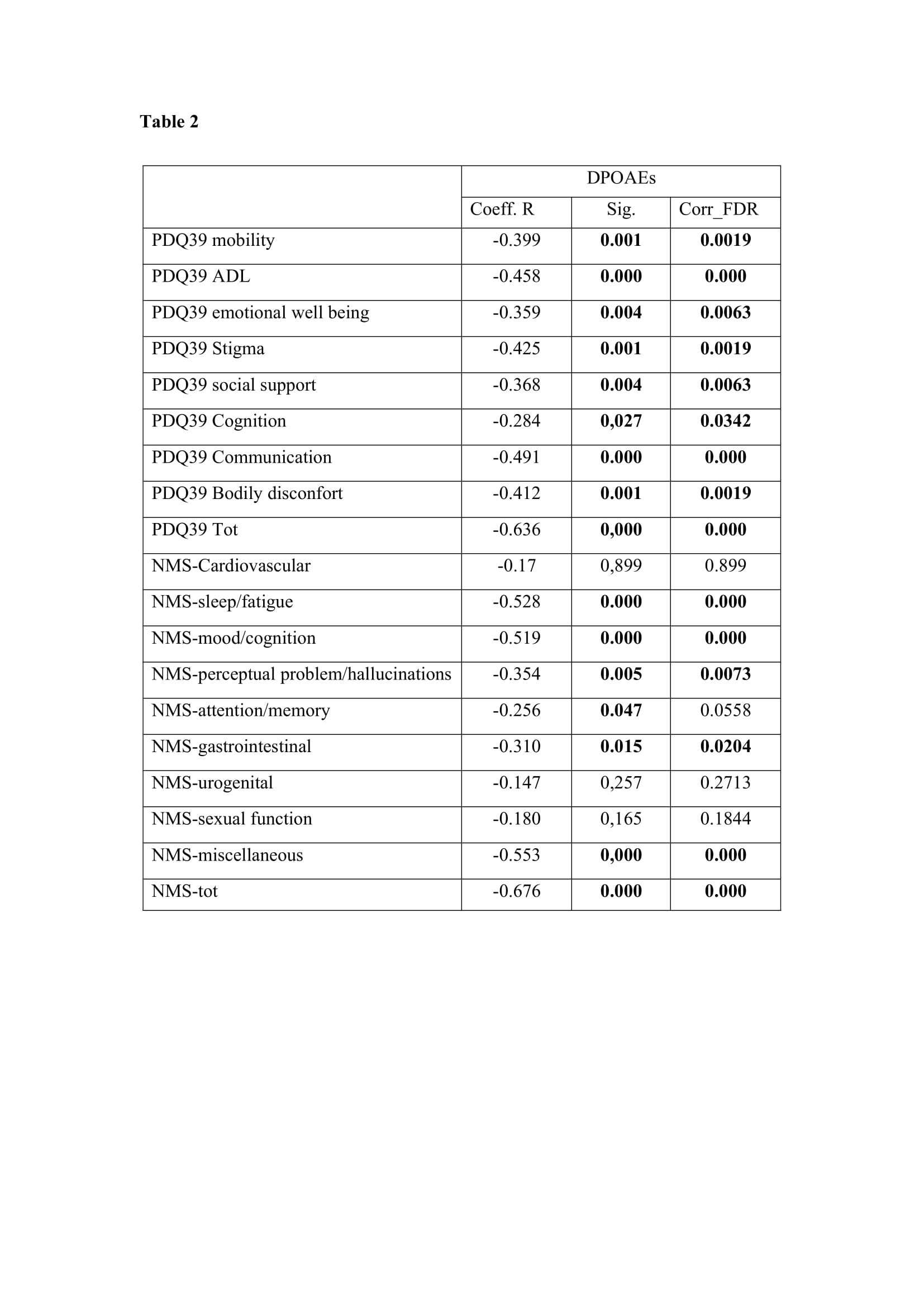
Results: We selected two cohort of patients, 59 who performed PTA (31 with hearing threshold >25dB and 28 lower than 25dB) and 64 with low signal-to noise ratio DPOAEs. Patients with HI had similar disease duration, UPDRS III and H&Y with respect to patients without HI, but were different for age and gender, being older and prevalently male. Concerning NMSS and PDQ39, patients with HI according to PTA, showed higher scores in almost all subdomain, with the main exception of cardiovascular (CV) and sexual function (SF) of NMSS. [table1] On the same trend, DPOAE variables showed significant correlation with age and every subdomain of the two scales (adjusted for age), except for NMS-CV, SF and urinary function (U). [table2]
Conclusion: This study demonstrated that PD patients with worst hearing function have a greater burden of NMS and lower related quality of life and functioning, regardless of disease staging and motor impairment. We supported the idea of PD being a systemic disease with multidomain involvement [3] . We pointed at reconsider HI as part of NMS and stress the importance of hearing evaluation, even in asymptomatic patients.
References: [1] Sisto R, Viziano A, Stefani A, Moleti A, Cerroni R, Liguori C, Garasto E, Pierantozzi M. Lateralization of cochlear dysfunction as a specific biomarker of Parkinson’s disease. Brain Commun. 2020 Sep 18;2(2):fcaa144.
[2] Vitale C, Marcelli V, Allocca R, Santangelo G, Riccardi P, Erro R, et al. Hearing impairment in Parkinson’s disease: Expanding the nonmotor phenotype. Mov Disord. 2012;27(12):1530–5.
[3] Titova N, Padmakumar C, Lewis SJG, Chaudhuri KR. Parkinson’s: a syndrome rather than a disease? J Neural Transm. 2017;124(8):907–14.
To cite this abstract in AMA style:
E. Garasto, M. Conti, A. Viziano, A. Stefani, M. Pierantozzi, NB. Mercuri, A. Moleti, R. Sisto, T. Schirinzi, R. Cerroni. Hearing impairment and non-motor symptoms in Parkinson’s disease: association and impact on quality of life [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/hearing-impairment-and-non-motor-symptoms-in-parkinsons-disease-association-and-impact-on-quality-of-life/. Accessed April 20, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/hearing-impairment-and-non-motor-symptoms-in-parkinsons-disease-association-and-impact-on-quality-of-life/