Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: To analyze the consistency of neural connections of the primary gustatory cortex (PGC), ranging from control group to progressive stages of Parkinson’s Disease (PD).
Background: Dysgeusia, as a non-motor symptom of PD, has not been established as strongly as olfactory dysfunctions have. Multiple studies state that dysgeusia has been noted uniformly in PD patients, but certain studies also state that taste acuity is seen to be enhanced in these patients. Such patients experienced a more intense response to gustatory stimuli of low concentration as compared to control groups. Three studies have presented statistically significant results to support that taste impairments and disease progression are associated. However, its consistency and clinical utility remain under scrutiny. It has been stated that dysgeusia noted in PD patients is not related to the disease itself but is a result of olfactory loss which leads to decreased gustatory function and trigeminal functions. This encouraged us to conduct a comparative study of neural connections of the PGC and regions associated with conveying and processing of gustatory stimuli between a control group and PD affected group and between the progressive stages of PD.
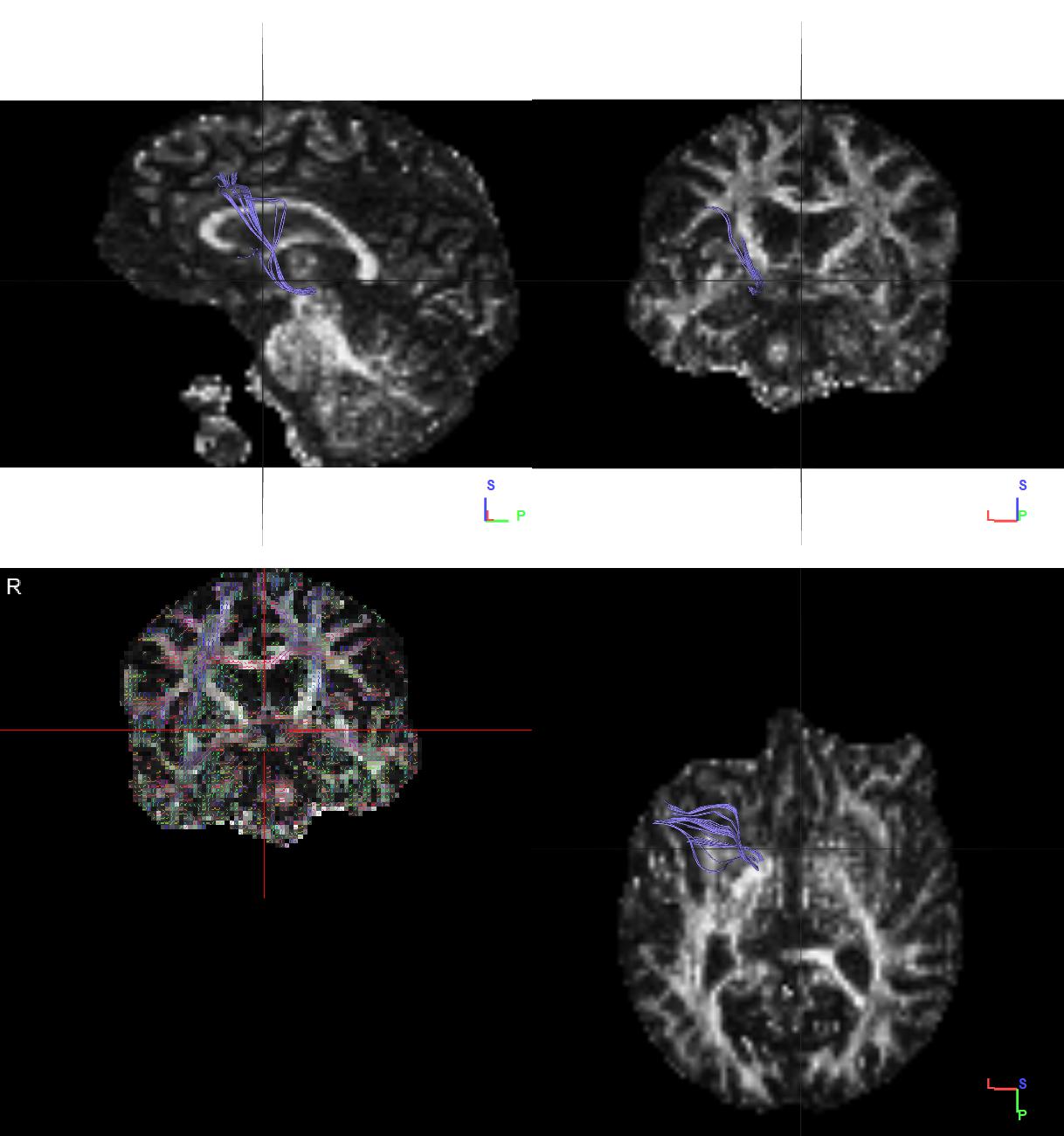
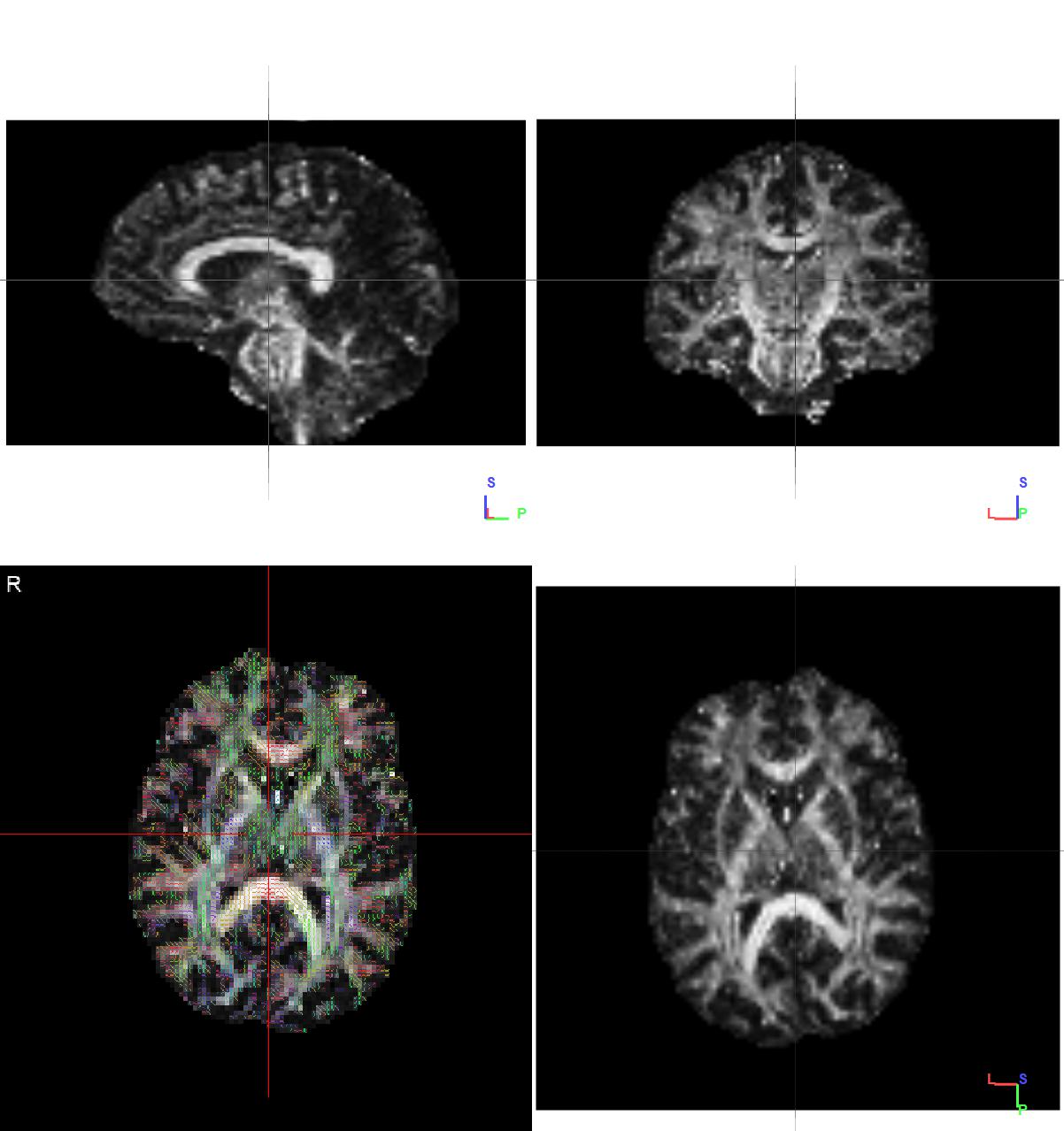
Method: Using fibre tractography on structural Magnetic Resonance Imaging (MRI) scans, we observed the number, length and volume of fibres connecting PGC with other regions. Comparisons were made among 4 groups, each group containing 40 MRI scans obtained from different individuals, one control group and three PD affected groups of spaced stages of progression.
Results: A statistically significant difference in fibres was noted between control and PD affected groups (figure 1&2), with a p-value of 0.0008, but difference noted in fibres among different stages of progression was not significant. In most PD affected MRIs the number of fibres noted was as low as zero.
Conclusion: From the results observed, we may derive that while there is a significant decrease in the fibres in PD affected group and we may conclude that PD does affect gustatory functions, there is a very little decline in fibres from initial stages to advanced stages. Therefore, although we may use monitoring of gustatory neural connections as a form of preliminary diagnosis, it may not serve the purpose of progression monitoring. However, in order to confirm the same, a similar study using functional MRI scans instead of structural MRI scans may provide better insight.
References: [1] Pritchard TC., et al. Taste Perception in Patients With Insular Cortex Lesions. Behavioral Neuroscicnce 1999. Vol. 113. No. 4. 663-671. [2] Goncalves CVF. Dysgeusia in Parkinson’s Disease: A Systemic Review. Faculdade de Medicina da Universidade de Coimbra. April 2016. [3] Kashihara K., et al. Frequency and characteristics of taste impairment in patients with Parkinson’s disease: results of a clinical interview. Intern Med. 2011;50(20):2311-5.
To cite this abstract in AMA style:
H. Chatterjee, G. Elumalai, N. Sewram, N. Osakwe. Gustatory Connectivity in Parkinson’s Disease Progression [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/gustatory-connectivity-in-parkinsons-disease-progression/. Accessed February 6, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/gustatory-connectivity-in-parkinsons-disease-progression/