Session Information
Date: Tuesday, September 24, 2019
Session Title: Dystonia
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To describe single unit neural activity in globus pallidus (GP) of cervical dystonia (CD) patient with putaminal stroke and compare it with CD patients without evidence of structural brain lesion.
Background: Previous studies have demonstrated that lesions in the posterior putamen and GPe might affect direct and indirect pathway of movement and induce dystonia [1,2]. Precise mechanisms of these effects have not been fully characterized.
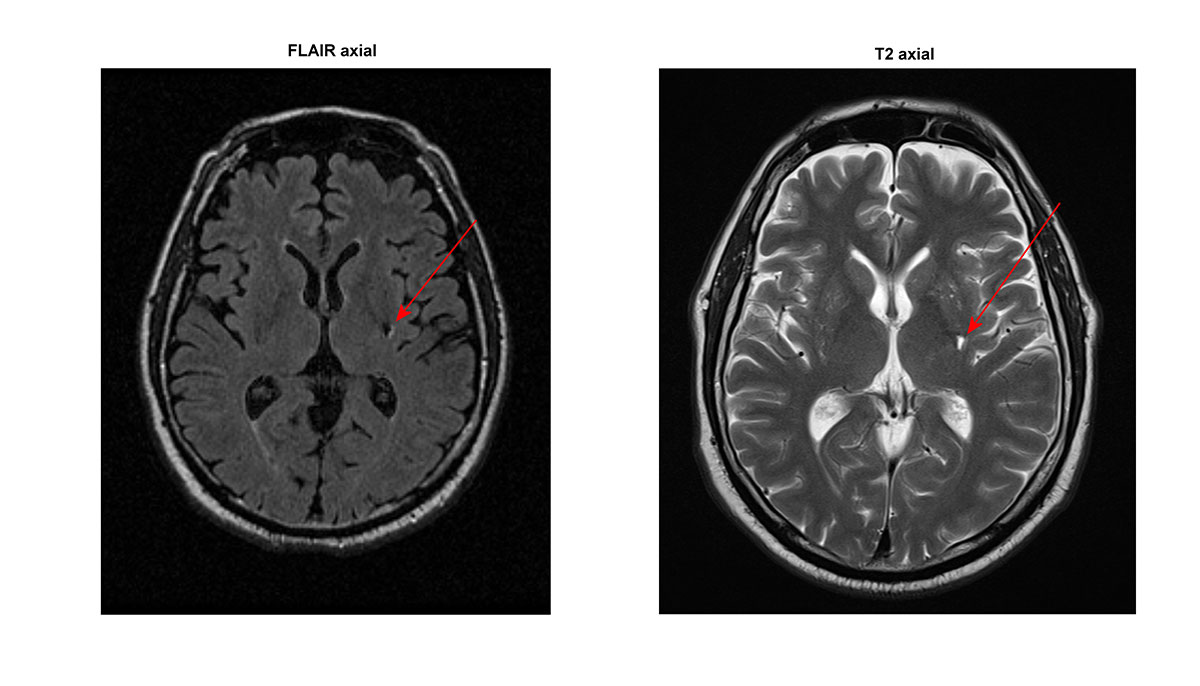
Method: A 48-year old man suffered ischemic stroke in July 2012 which manifested as right-side hemiparesis, right facial weakness, and aphasia. The symptoms regressed in 4 months, although MRI revealed a lacunar poststroke lesion in left posterior putamen [figure1]. 10 months later patient developed CD with predominant right-side torticollis. He was repeatedly treated with botulinum toxin, however, no relief in dystonia or pain was achieved. At the age of 54, he was evaluated for bilateral GPi-DBS. We used intraoperative microelectrode recording during implantation of the electrodes. We analyzed firing rate (FR) and coefficient of variance (CV) in GPi and GPe and compared them with parameters of 6 CD patients with robust torticollis.
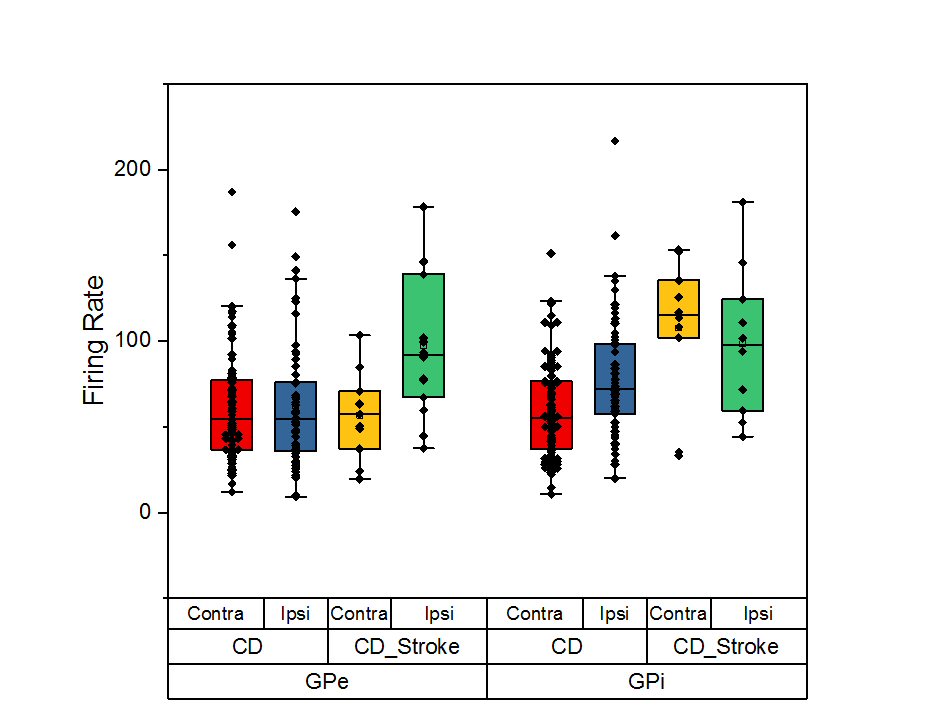
Results: In CD patient with putaminal stroke, neural activity was characterized by high frequency regular discharges (FR>100 imp/sec in GPi and FR>70 imp/sec in GPe, CV<1). CD patients without lesions in basal ganglia were characterized by relatively low frequency (FR 50-60 imp/sec) and irregular or burst-like discharge pattern (CV>1.2), p<0.01. We also saw robust asymmetry in GPe FR (p<0.01) and no significant differences in GPi FR in CD patient with poststroke putaminal lesion. In contrast, other CD patients showed asymmetry in GPi and no asymmetry in GPe [figure2]. We switched on GPi-DBS separately for each lead. Significant amelioration in CD was achieved only by activation of the electrode ipsilateral to direction of head rotation (58.3% in motor TWSTRS).
Conclusion: Electrophysiological characteristics of GP neural activity in a CD patient with putaminal cyst significantly differ from CD patients with normal MRI. These findings suggest possible pathogenetic relationship between lesion in posterior putamen and appearance of delayed cervical dystonia. Moreover, imbalance in the neck proprioceptive feedback might contribute to pallidal asymmetry [3]. Study was funded by the Russian Science Foundation (project 18-15-00009).
References: 1. Vidailhet, M., Grabli, D., & Roze, E. (2009). Pathophysiology of dystonia. Current opinion in neurology, 22(4), 406-413. 2. Park J. (2016). Movement Disorders Following Cerebrovascular Lesion in the Basal Ganglia Circuit. Journal of movement disorders, 9(2), 71-9. 3. Sedov, A., Usova, S., Semenova, U., Gamaleya, A., Tomskiy, A., Crawford, J. D., … & Shaikh, A. G. (2019). The role of pallidum in the neural integrator model of cervical dystonia. Neurobiology of disease.
To cite this abstract in AMA style:
A. Gamaleya, A. Tomskiy, S. Usova, V. Popov, AG. Shaikh, A. Sedov. Features of neural activity of globus pallidus in a patient with cervical dystonia and putaminal stroke: case study [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/features-of-neural-activity-of-globus-pallidus-in-a-patient-with-cervical-dystonia-and-putaminal-stroke-case-study/. Accessed December 28, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/features-of-neural-activity-of-globus-pallidus-in-a-patient-with-cervical-dystonia-and-putaminal-stroke-case-study/