Category: Technology
Objective: Determine incidence of falls in a group of PD patients and correlate their clinical characteristics with parameters of gait kinetics obtained through videos recorded with a smartphone.
Background: Postural and gait impairments in Parkinson’s Disease (PD) are a major challenge due to superposition of body changes attributed to aging itself and biomechanical variations determined by PD and its compensatory mechanisms. (1–3) The use of technology-based objective measures (TOMs) in clinical practice is an expanding reality, however, its popularization is limited by difficulty of access, lack of standardization in interpretation of the data obtained and high cost. (4–6)
Method: Cross-sectional evaluation of demographic, clinical data and quantitative gait analysis using kinematics. We recorded videos of the patients’ straight gait, walking at normal speed, for 6 meters, with an IPhone XS with 4K resolution at 60 frames/second. Smartphone was fixed at a distance of 6 meters from the target, with a right-side view of the patients, for analysis of gait in the sagittal plane. We used the simple anatomical model to determine the position of the joints for later capture of gait kinetics variables using the free two-dimensional kinematic analysis software, CvMob. (7,8)
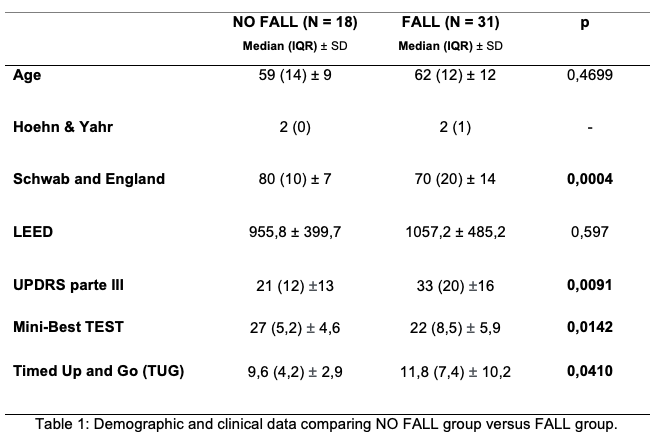
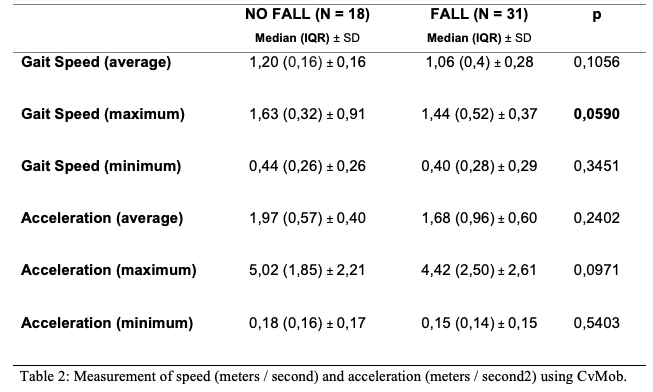
Results: We evaluated 49 PD patients, predominantly male (67%) with average age of 59 years (±10,9). 63,2% of patients experienced at least one fall episode in the last year and 86% experienced a near-fall situation. Patients with fall history have higher score at UPDRS-III, higher TUG and worst performance in MiniBestTEST (Table 1). We used a smartphone as an auxiliary tool to capture data of gait kinetics with an easily reproducible and low operating cost model. Our data suggest that objective measure of maximum speed, extracted through the analysis of the smartphone-video by CvMob, tended to serve as a marker of risk of falls in PD patients (Table 2).
Conclusion: Maximum gait speed, in our series, tended to serve as a marker for identifying patients at risk of falls. We used an easily, reproducible and low operational cost model to determinate gait parameters using a smartphone. This allows new studies to be carried out with larger populations to analyze broader data of gait kinetics and identify changes in posture, balance and gait characteristics capable of predicting increased risk of falls.
References: 1. Wilson J, Alcock L, Yarnall AJ, Lord S, Lawson RA, Morris R, et al. Gait Progression Over 6 Years in Parkinson’s Disease: Effects of Age, Medication, and Pathology. Front Aging Neurosci [Internet]. 2020 Oct 15;12. Available from: https://www.frontiersin.org/article/10.3389/fnagi.2020.577435/full 2. Galna B, Lord S, Burn DJ, Rochester L. Progression of gait dysfunction in incident Parkinson’s disease: Impact of medication and phenotype. Mov Disord. 2014;30(3):359–67. 3. Lima DP, de Almeida SB, de Carvalho Bonfadini J, de Luna JRG, de Alencar MS, Pinheiro-Neto EB, et al. Clinical correlates of sarcopenia and falls in Parkinson’s disease. PLoS One. 2020;15(3):1–12. 4. Merola A, Sturchio A, Hacker S, Serna S, Vizcarra JA, Marsili L, et al. Technology-based assessment of motor and nonmotor phenomena in Parkinson disease. Vol. 18, Expert Review of Neurotherapeutics. Taylor and Francis Ltd; 2018. p. 825–45. 5. Arora S, Venkataraman V, Zhan A, Donohue S, Biglan KM, Dorsey ER, et al. Detecting and monitoring the symptoms of Parkinson’s disease using smartphones: A pilot study. Park Relat Disord [Internet]. 2015;21(6):650–3. Available from: http://dx.doi.org/10.1016/j.parkreldis.2015.02.026 6. Peña N, Cecílio Credidio B, Peixoto L, Rodriguez N, Salles Corrêa M, Souza França LG, et al. Free instrument for measurements of motion. Rev Bras Ensino Física. 2013;35(3):3505 1-5. 7. Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: Evidence and implications. Mov Disord. 2013;28(11):1520–33. 8. Custodio N, Lira D, Herrera-Perez E, Montesinos R, Castro-Suarez S, Cuenca-Alfaro J, et al. Predictive model for falling in Parkinson disease patients. eNeurologicalSci. 2016;5:20–4. 9. Kerr GK, Worringham CJ, Cole MH, Lacherez PF, Wood JM, Silburn PA. Predictors of future falls in Parkinson disease. Neurology. 2010;75(2):116–24. 10. McKay JL, Hackney ME, Factor SA, Ting LH. Lower Limb Rigidity Is Associated with Frequent Falls in Parkinson’s Disease. Mov Disord Clin Pract. 2019;6(January):446–51. 11. Espay AJ, Bonato P, Nahab FB, Maetzler W, Dean JM, Klucken J, et al. Technology in Parkinson’s disease: Challenges and opportunities. Mov Disord. 2016;31(9):1272–82.
To cite this abstract in AMA style:
F. Rolim, A. Gomes, E. Barreto, A. Marinho, F. Carvalho. FEASIBILITY OF A SMARTPHONE-BASED APPROACH TO ACCESS GAIT PARAMETERS AND DETECT FALL RISK IN PARKINSON’S DISEASE [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/feasibility-of-a-smartphone-based-approach-to-access-gait-parameters-and-detect-fall-risk-in-parkinsons-disease/. Accessed December 31, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/feasibility-of-a-smartphone-based-approach-to-access-gait-parameters-and-detect-fall-risk-in-parkinsons-disease/