Category: Spasticity
Objective: The comprehensibility, feasibility, and appraisal of the Spastic Movement Disorders Decision Tree (SMD-DT) was assessed by qualitative analysis of study feedback collected from raters with different professional background. The raters’ demographic and professional profiles were described.
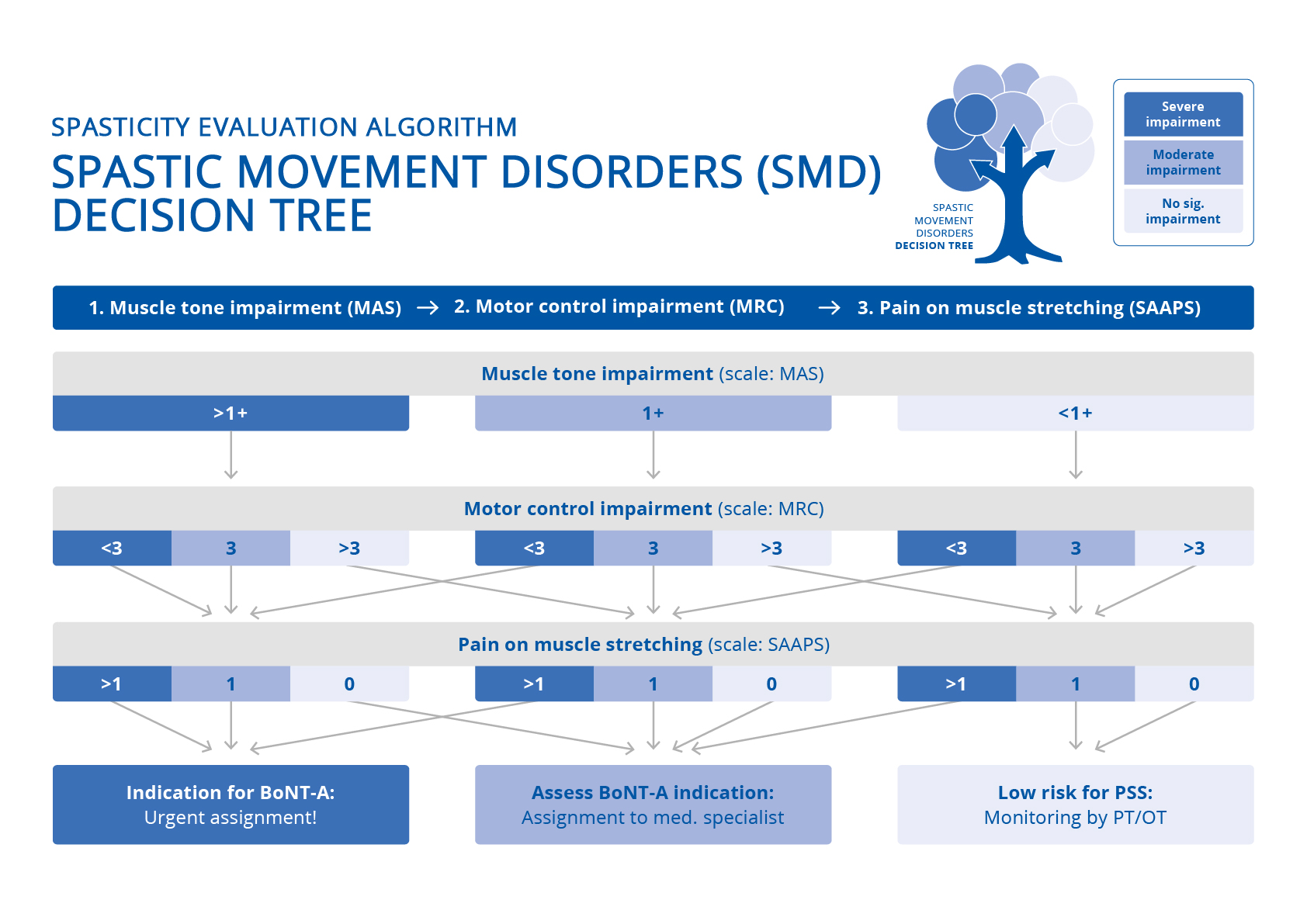
Background: The SMD-DT, a tool assessing muscle tone, control of voluntary movements and pain, was developed for early recognition of potential disabling spasticity [1]. An initial validation study with post-stroke patients suggested a straight-forward and time-efficient use of the SMD-DT (I-REFER [2]).
Method: Data on demographic and professional profiles of the raters (nurses, physio- and occupational therapists) during 4 I-REFER validation study days with n=69 post-stroke patients were recorded. Per study day, 2 therapists and 2 nurses rated patients’ needs for assigning to focal spasticity treatment using the SMD-DT (study design: see Fheodoroff et al. (2024) [2].
Raters feedback on ease of use, (dis-)advantages of the SMD-DT and relevance to their work was collected.
Results: 5 nurses and 4 therapists (2 occupational and 2 physiotherapists) contributed to this qualitative analysis. Average age was 33.3 (24-47) years and average professional experience was 9.3 (2-25) years. 1 nurse and 2 therapists hold a BSc. 6 of 9 raters obtained additional qualifications in special neurology care and/or kinaesthetics. Examination time per PSS patient using the Decision Tree was reported between 5 min for straight-forward and 10 min for more complex patients. Average examination time decreased with each performance.
The SMD-DT was perceived as user-friendly and practical. Therapists valued the streamlined patient assessment, while nurses appreciated their role in documenting and facilitating communication about patients’ mobility and care issues with the multidisciplinary team members. Both, nurses and therapists endorsed its use in routine care.
Therapists who previously used the original scales used in the SMD-DT reported mild difficulties in using the simplified scales. Nurses felt somewhat insecure due to lack of experience in structured assessment of PSS.
Conclusion: Both, nurses and therapists considered the SMD-DT a useful tool in examining post-stroke patients for potential spastic movement disorders that may require BoNT/A treatment by a skilled specialist.
SMD Decision Tree
References: [1] WCNR 2022, Vienna Poster #P101 – Presented at the 12th WCNR in Vienna on Dec. 15th, 2022
[2] Fheodoroff, K., Waeschle, B., & Wissel, J. (2024). Initial Assessment of the Validity and Inter-Rater Reliability For Early Recognition of Spasticity Using the Decision Tree Tool (I-REFER). Toxicon, 237(Supplement 1), 107399
To cite this abstract in AMA style:
K. Fheodoroff, B. Waeschle, J. Wissel. Feasibility and Comprehensibility of the SMD Decision Tree for Early Recognition of Spasticity [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/feasibility-and-comprehensibility-of-the-smd-decision-tree-for-early-recognition-of-spasticity/. Accessed December 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/feasibility-and-comprehensibility-of-the-smd-decision-tree-for-early-recognition-of-spasticity/