Session Information
Date: Tuesday, June 6, 2017
Session Title: Technology
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: To compare the efficacy of five smartphone-enabled active tests in detecting severity changes after medication, via an automated Parkinson Disease Severity Score (PDSS).
Background: Traditional severity metrics such as UPDRS provide low-resolution assessments that can only be collected by physicians in clinic. Self-administered active tests via smartphone provide a new way to monitor the granular progression of PD severity on a daily basis out of clinic.
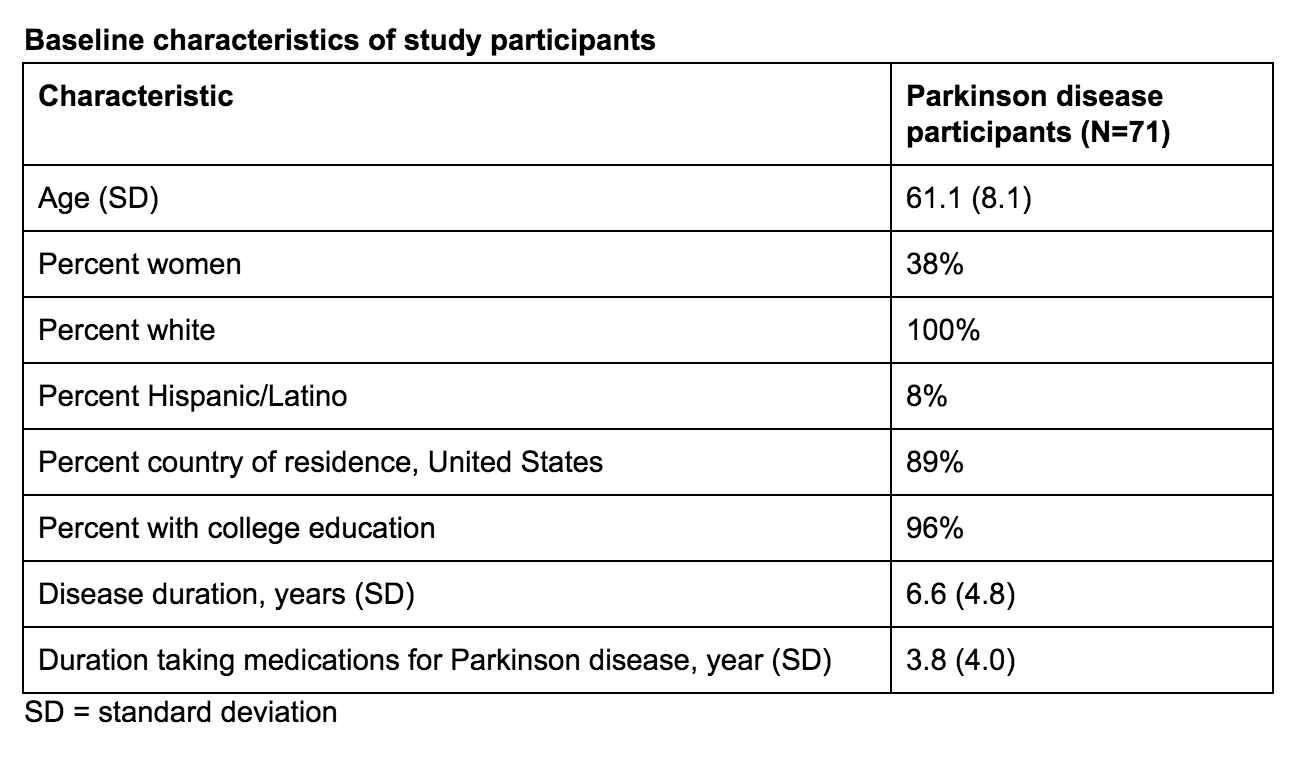
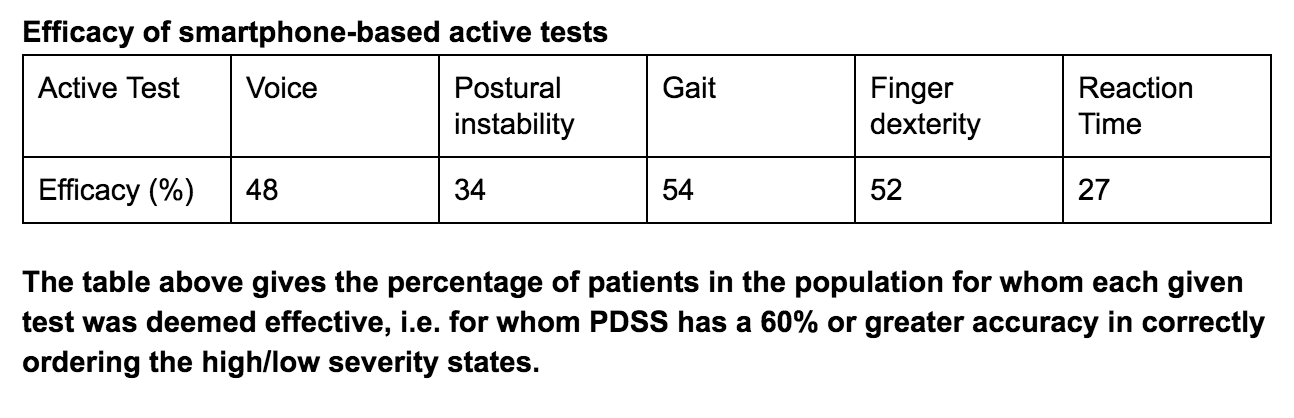
Methods: Using the HopkinsPD app [2], 71 individuals on medication (Table 1) record measurements from 5,800 self-administered active tests in pairs — right before and within one hour after their first dose — to measure aspects of motor function such as voice, postural instability, gait, finger dexterity, and reaction time. A novel machine learning algorithm for disease severity score learning (DSSL) [1] is used to train five models that map this vector of measurements to a scalar severity score, the PDSS. The algorithm assumes that the severity ordering, before and after medication, is correct in the majority of training examples provided. 10-fold cross validation is used to evaluate model performance, under the assumption that no individual appears in both the train set and test set. Model accuracy is defined to be the ratio of active tests in which PDSS decreases after the first dose. An active test is labeled effective if it is at least 60% accurate.
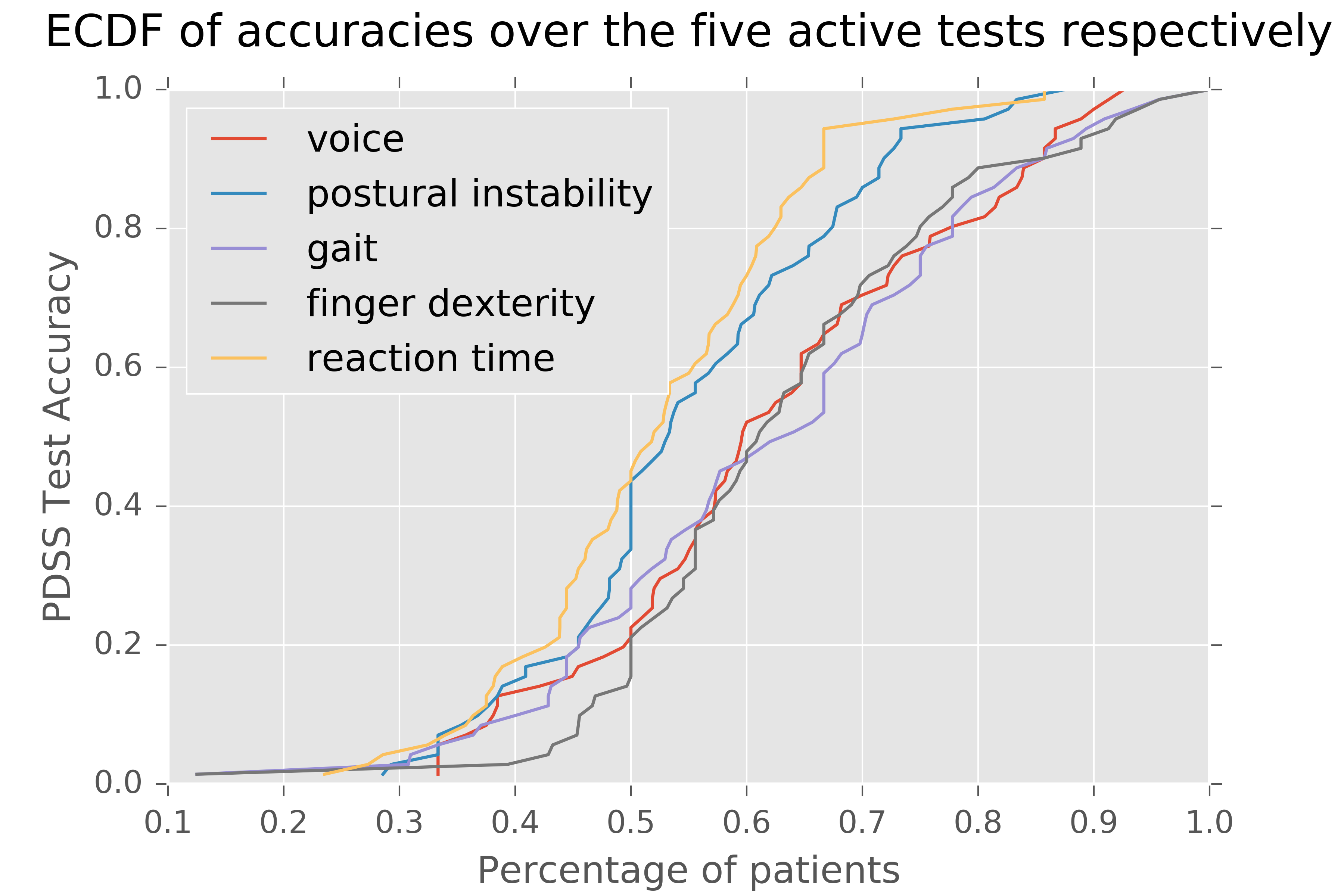
Results: 89% and 69% of the population had at least one and two effective active tests, respectively. Both the gait and finger dexterity tests — the two most informative tests — are effective in more than half of all subjects (Table 2). 17% of patients for whom 3 or more individual tests were effective had long-standing disease duration, with a mean of 8.8 years. The 11% of patients for whom no active test was effective all had short medication histories of less than five years. Across the voice, finger dexterity, and gait tests, PDSS was at least 70% accurate on between 30% and 40% of patients (Figure 1).
[table1]
[table2]
[figure1]
Conclusions: That PDSS, generated from measurements in smartphone-enabled active tests, is effective in tracking motor fluctuations for at least half of the population in close to 3 of 5 active tests is promising. It warrants further investigation into the feasibility of automated severity scoring in monitoring the short-term and long-term variation of PD severity.
References: [1] D. Kirill, and S. Saria. “Learning (predictive) risk scores in the presence of censoring due to interventions.” Machine Learning 102.3 (2016): 323-348.
[2] A. Zhan, MA Little, DA Harris, SO Abiola, E Dorsey, S. Saria, and A. Terzis, “High Frequency Remote Monitoring of Parkinson’s Disease via Smartphone: Platform Overview and Medication Response Detection”, arXiv preprint arXiv:1601.00960, 2016.
To cite this abstract in AMA style:
A. Zhan, S. Mohan, M. Elson, E. Dorsey, A. Terzis, S. Saria. Efficacy of Smartphone-enabled Active Tests in Automated PD Severity Assessment [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/efficacy-of-smartphone-enabled-active-tests-in-automated-pd-severity-assessment/. Accessed December 14, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/efficacy-of-smartphone-enabled-active-tests-in-automated-pd-severity-assessment/