Category: Parkinson's Disease: Pathophysiology
Objective: We investigated the effects of multi-strain probiotics administration on gut microbiome and metabolites, and markers of intestinal permeability and inflammation.
Background: Probiotics have been shown to improve constipation in Parkinson’s disease (PD), however, its mechanisms of action remain to be elucidated.
Method: Fecal and serum samples were collected from 47 subjects participating in a double-blind placebo-controlled trial (multi-strain probiotics capsules, n=24; placebo, n=23), prior to and 4 weeks after intervention. Gut microbiome was analyzed using 16S rRNA gene sequencing; fecal short-chain fatty acids (SFCAs) using gas chromatography; and serum zonulin and fecal calprotectin (markers of intestinal permeability and inflammation, respectively) using enzyme-linked immunosorbent assay. Fecal gene abundance for tyrosine decarboxylase (tdc; a microbial enzyme implicated in levodopa metabolism) was quantified via real-time polymerase chain reaction using primers TYR3f and TYR4r.
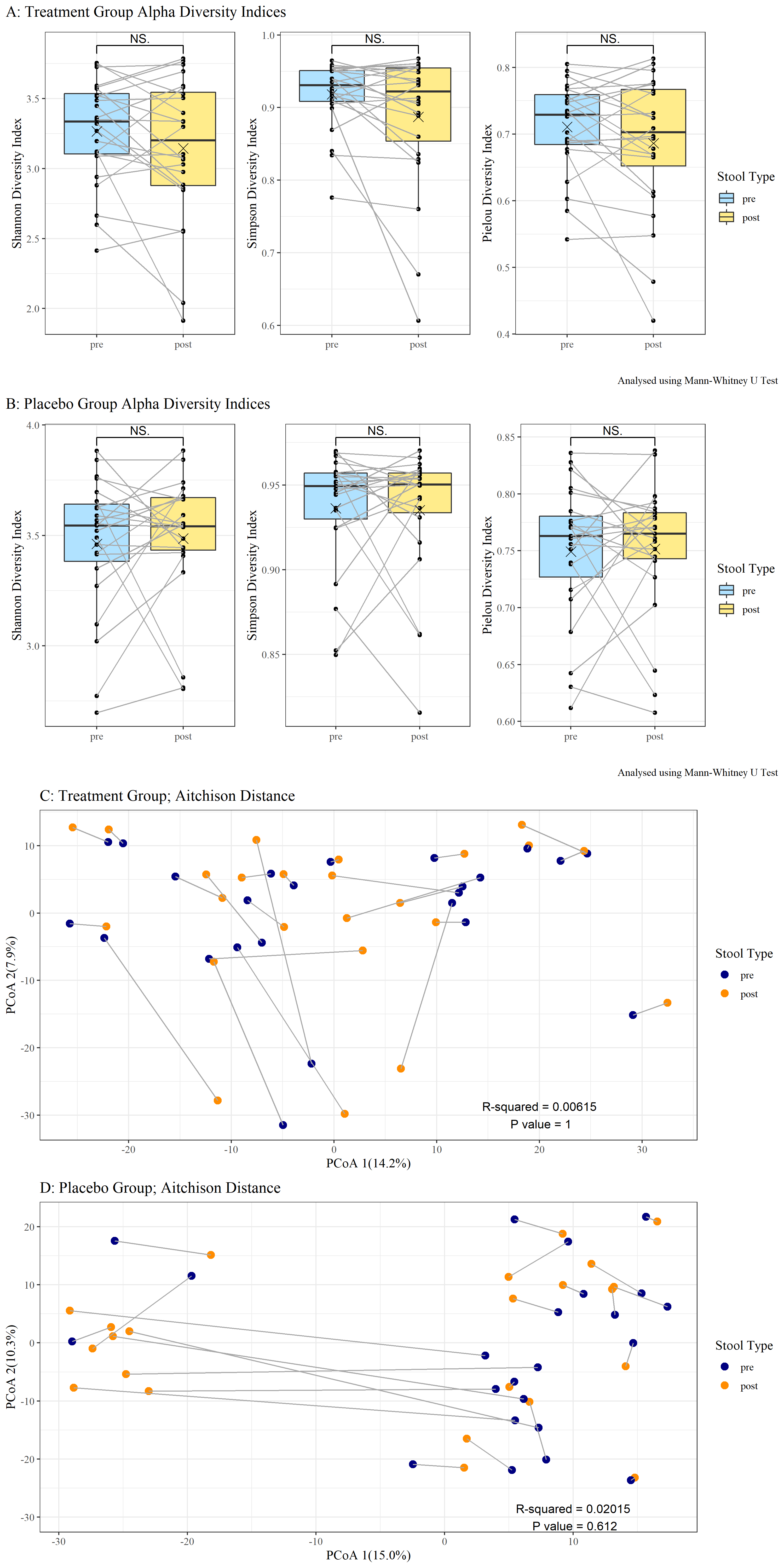
Results: There were no significant changes in gut microbiome composition (i.e., alpha and beta diversity indices, temporal variability, and differential abundances of microbial taxa) before and after intervention in both groups (Figure 1). Probiotics administration was associated with increased fecal acetate (0.0970[0.0369] vs. 0.0750[0.0430] nmol/g, p=0.026), but not propionate or butyrate. These fecal SCFAs did not change significantly in the placebo group. Serum zonulin, fecal calprotectin and fecal tdc abundance did not change significantly pre- and post-intervention in both groups. Interestingly, higher fecal acetate correlated with lower/better Hoehn and Yahr and MDS-UPDRS parts II and III scores. The abundance of fecal tdc correlated with several microbial taxa, but no correlations were found between microbial taxa and fecal SCFAs, fecal calprotectin, or serum zonulin.
Conclusion: Our findings suggest that probiotics administration may augment potentially beneficial gut metabolites such as fecal acetate in PD patients, but without altering gut microbial composition. Longer-term clinical trials with sequential analyses of gut markers, and pre-clinical models will improve our understanding of the therapeutic and mechanistic effects of probiotics in PD.
To cite this abstract in AMA style:
JW. Hor, SY. Lim, CW. Chong, SL. Song, CSJ. Teh, TS. Toh, JL. Lim, KY. Khaw, AH. Tan. Effect of multi-strain probiotics on gut microbiome and metabolites in Parkinson’s Disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/effect-of-multi-strain-probiotics-on-gut-microbiome-and-metabolites-in-parkinsons-disease/. Accessed April 20, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/effect-of-multi-strain-probiotics-on-gut-microbiome-and-metabolites-in-parkinsons-disease/