Session Information
Date: Monday, September 23, 2019
Session Title: Rare Genetic and Metabolic Diseases
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To extend the spectrum of clinical phenotype in the alacrima, achalasia and mental retardation syndrome(AAMR) by reporting a case.
Background: AAMR is a newly described rare autosomal recessive disorder characterized by alacrima, achalasia and mental retardation usually in early life caused by mutation in the guanosine diphosphate (GDP)-mannose pyrophosphorylase A(GMPPA) gene.To date, only 18 cases had been reported.Most cases share the three main features.Less frequently phenotype includes hypotonia, gait abnormalities and visual/hearing impairment.To better clarify the spectrum of the disease and further recognize genotype-phenotype correlations of this syndrome,detailed phenotypic reports of new cases with AAMR, as well as new deleterious mutations are in demand
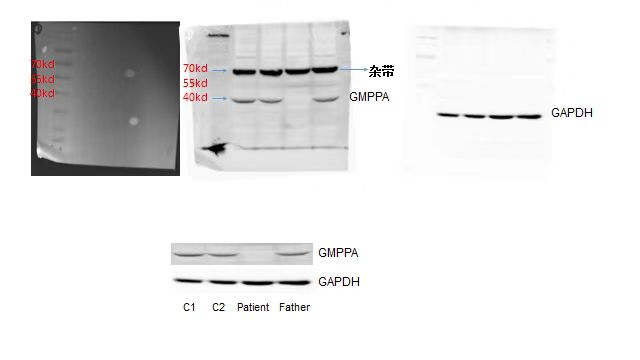
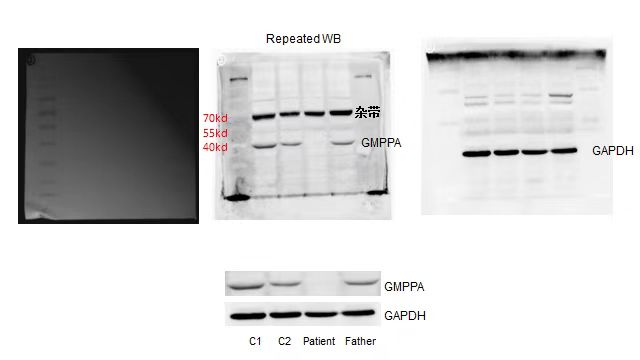
Method: A 27-year-old Chinese woman presented with bilateral tremor for 18 years,aggravating abnormal gesture in trunk and neck for 1 year.Feeding difficulties and frequent vomiting was noted after a normal full-term birth.Delayed mental development,speech delay and short stature were present. At 7 years old,she was found to have achalasia and received operation with partial remission of vomiting.No family history was presented.Protruding chin,sparse hair,a short philtrum,downturned corners of the mouth and scoliosis were present.Neurological Examination showed cognitive decline(MMSE23,MoCA12),dystonia involving craniofacial segment,four limbs and trunk.No other abnormal signs were present.She had xeroma assessing by tear breaking-time(BUT), fluorescein staining (FS) and Schirmer test. Other tests such as organic acids,ceruloplasmin,blood smear,autoimmune antibodies and brain MR were normal.As alacrima, achalasia and mental retardation were present, AAMR was suspected.GWAS was performed and showed novel homozygous missense mutation in GMPPA c.377T>C(p.Met126Thr). Western blot of cells from the patient showed absence of GMPPA compared with controls. As no gene mutations associated with dystonia were found,it’s reasonable to regard dystonia as a new phenotype of AAMR. DBS surgery was performed and relieved most of dystonia in 1 month.Long term follow-up is needed to evaluate further effects.
Results: We diagnose the patient as AAMR and dystonia related to GMPPA confirmed by gene testing with good response to DBS.
Conclusion: Dystonia could be a clinical symptom of AAMR related to GMPPA mutation and would respond to DBS.
References: 1. Koehler K, et al. Am J Hum Genet. 2013 Oct 3;93(4):727-34. 2. Benítez EO,et al. Mol Syndromol. 2018 Feb;9(2):110-114.
To cite this abstract in AMA style:
SL. Li, H. Wang, L. Wang, Y. Guo, XH. Wan, HP. Li, JY. Shi. Dystonia as a main clinical feature of AAMR with a novel GMPPA mutation:A case report [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/dystonia-as-a-main-clinical-feature-of-aamr-with-a-novel-gmppa-mutationa-case-report/. Accessed April 22, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/dystonia-as-a-main-clinical-feature-of-aamr-with-a-novel-gmppa-mutationa-case-report/