Session Information
Date: Sunday, October 7, 2018
Session Title: Epidemiology
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
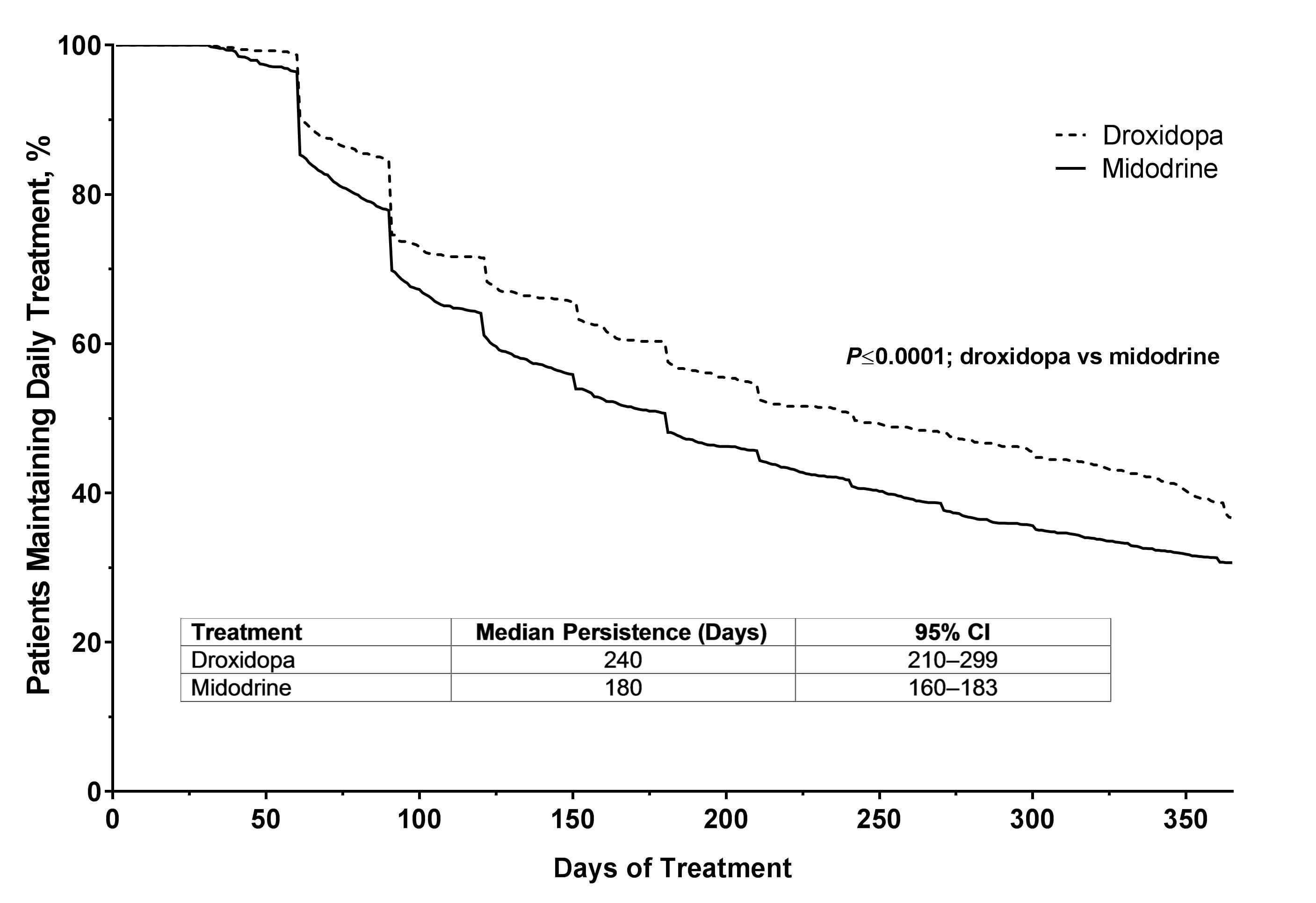
Objective: To determine the treatment persistence of droxidopa and midodrine in patients with orthostatic hypotension (OH) or neurogenic orthostatic hypotension (nOH) when medication cost was not a factor
Background: nOH is a sustained drop in blood pressure upon standing with a neurogenic etiology that can lead to falls, impaired function, and poor quality of life. The US Food and Drug Administration has approved droxidopa and midodrine in adults to treat symptomatic nOH and symptomatic OH, respectively. We compared treatment persistence over 1 year in patients not responsible for a copay taking droxidopa or midodrine.
Methods: Retrospective data on patients prescribed either droxidopa or midodrine were collected from the Symphony Health Solutions Database (Symphony Health; Conshohocken, PA, USA). Inclusion criteria were continuous healthcare coverage from Sept 1 2014, to June 30 2017, an active prescription for droxidopa or midodrine of ≥30 days’ duration in that same window, and no copay ($0.00) for the prescribed drug. Persistence was capped at 365 days to provide an unbiased comparison between midodrine (introduced in 1996) and droxidopa (introduced in 2014). The statistical difference between estimated survival curves for droxidopa and midodrine was calculated using a log-rank test and a multivariable Cox regression analysis.
Results: Treatment persistence data from 688 patients on droxidopa (mean ± SD age, 63.8±16 years; 48% women) and 1888 patients on midodrine (55.2±16 years; 62% women) were included. Of the patients on droxidopa, 12% had a diagnosis of Parkinson disease (PD), 34% cardiovascular disease (CVD), 18% both PD and CVD, and 35% unknown. Of the patients on midodrine, 1% had a diagnosis of PD, 69% CVD, 3% both PD and CVD, and 26% unknown. Median persistence was significantly longer for droxidopa (240 days; 95% confidence interval [CI], 210–299]) compared with midodrine (180 days; 95% CI, 160–183; P<0.0001; figure1). After adjusting for imbalances in demographic and clinical factors using Cox regression, patients on midodrine were 27.4% more likely to become non-persistent than those on droxidopa (P=0.002). [figure1]
Conclusions: When medication cost is not an influencing factor due to insurance coverage, patients using droxidopa were more likely to remain on treatment than patients on midodrine. The reason for this is unknown, but could be due to enhanced efficacy or fewer side effects.
To cite this abstract in AMA style:
S. Kymes, K. Jackson, M. Widolff, C. Sullivan, L. Hewitt, S. Raj. Droxidopa and Midodrine Treatment Persistence in Patients with Orthostatic Hypotension [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/droxidopa-and-midodrine-treatment-persistence-in-patients-with-orthostatic-hypotension/. Accessed February 3, 2026.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/droxidopa-and-midodrine-treatment-persistence-in-patients-with-orthostatic-hypotension/