Session Information
Date: Monday, June 20, 2016
Session Title: Parkinsonism, MSA, PSP (secondary and parkinsonism-plus)
Session Time: 12:30pm-2:00pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: Clinical characterization of a tauopathy spectrum patient.
Background: In recent years phenotypic overlap has been demonstrated between patients with progressive supranuclear palsy (PSP) pathology and corticobasal degeneration (CBD) pathology. Dorsal simultanagnosia is a cortical deficit of visual attention that can rarely be found in CBD patients. In dorsal simultanagnosia copying a drawing is impaired.
Methods: We characterize a tauopathy spectrum patient.
Results: The patient presented at age 72 with balance problems leading to frequent falls. The DATscan was abnormal. After two years he developed word finding difficulties and agrammatism. At age 77 the progressive non-fluent aphasia (PNFA) phenotype still dominates. Examination shows a symmetric hypokinetic-rigid syndrome with abnormal postural reflexes, frontal release signs and a vertical supranuclear gaze palsy. Oral apraxia or a cortical sensory deficit could not be demonstrated. MRI findings suggest underlying PSP pathology with a hummingbird sign, a Mickey Mouse sign and superior cerebellar peduncle atrophy. The neuropsychological examination demonstrated abnormal executive functioning. Further language testing was concordant with a PNFA phenotype. On the Boston Naming test (BNT) and the Cookie theft picture this patient displayed dorsal simultanagnosia. When confronted with the “tree” picture he only saw “leaves”. He could impossibly master the complete Cookie theft scene. When copying figures, he omitted salient surface features and had a lack of perspective. The other features of Balint’s syndrome were lacking. 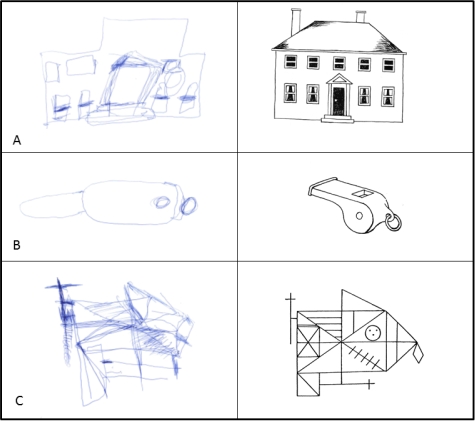 Fig. 1. Copying figure task. A.) The house of the BNT lacks its chimneys as a salient surface feature. B.) The whistle of the BNT has an incorrect perspective. C.) The Complex figure of Rey lacks important features. On the right the original figure is included.
Fig. 1. Copying figure task. A.) The house of the BNT lacks its chimneys as a salient surface feature. B.) The whistle of the BNT has an incorrect perspective. C.) The Complex figure of Rey lacks important features. On the right the original figure is included.
Conclusions: The patient meets the 2013 Armstrong criteria for probable CBD. However, the initial presentation and imaging is prototypical for Richardson’s syndrome. Thus, he can also be classified as PSP-CBS. To our knowledge, this is the first patient who presents with dorsal simultanagnosia in combination with PSP. This case poses a challenge for clinicians using the current diagnostic criteria for CBD and PSP. Our patient adds to the growing phenotypic spectrum of tauopathies.
To cite this abstract in AMA style:
B. Bergmans, O. Deryck, R. Bruffaerts. Dorsal simultanagnosia as a cortical sign in the tauopathy spectrum [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/dorsal-simultanagnosia-as-a-cortical-sign-in-the-tauopathy-spectrum/. Accessed April 20, 2025.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/dorsal-simultanagnosia-as-a-cortical-sign-in-the-tauopathy-spectrum/
