Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: To explore the impact of an anticholinergic burden on various outcomes in Parkinson’s disease.
Background: Over 600 different medications possess some anticholinergic effect.[1] There is a greater susceptibility to both peripheral and central adverse effects of anticholinergics in the elderly population.[2] Most people with Parkinson’s are aged >60,[3] whose risks are further increased by the presence of cholinergic dysfunction.[4]
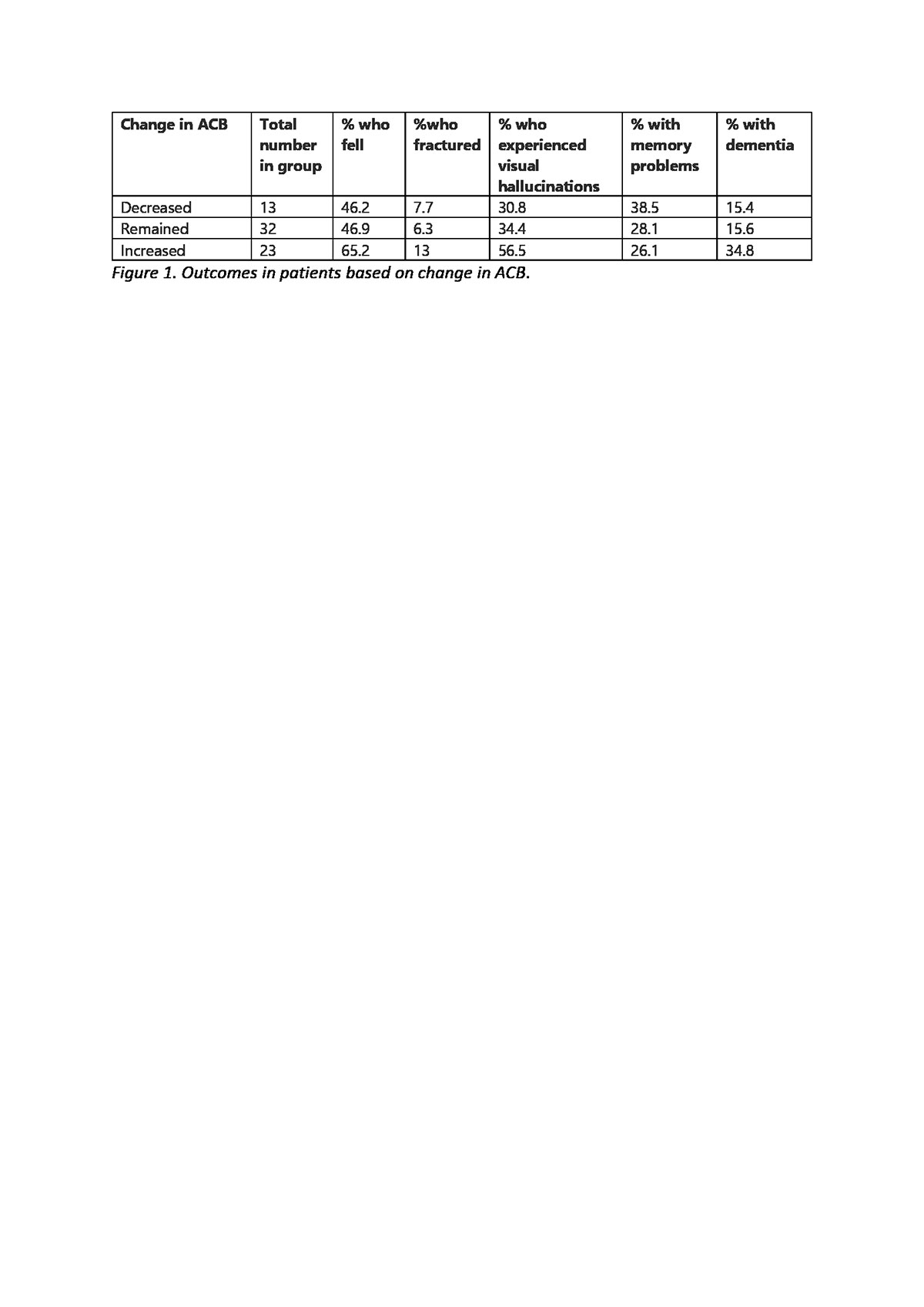
Method: Study population of 72 deceased patients previously diagnosed with Parkinson’s disease. 4 patients were excluded due to insufficient data. For the remaining 68, an anticholinergic burden score (ACB) was calculated at diagnosis and death. ACB was determined using the anticholinergic cognitive burden scale.[5] Several primary outcomes were then looked at for each patient [table1]. Survival (years) was a secondary outcome (measured in whole years). Patients were split into 3 groups based on baseline ACB: 0, 1 & ≥2 (maximum score of 7). The rate of primary outcomes and average survival was then determined for each group. This was repeated with a further 3 groups, based on whether a patient’s baseline ACB had decreased, remained the same or increased.
Results: No association was found between a higher ACB at baseline and the occurrence of any primary outcome. A trend was found between an increase in baseline ACB and several outcomes [table1]. Survival was lowest for those with an ACB of ≥2 at baseline (1.6 years). However, those with an increase in ACB over baseline had greater average survival (2.5 years). For groups at baseline and change in ACB, a chi-sqaured statistic was calculated for all outcomes except average survival, where a log rank test was performed. All p-values calculated were >0.05. Therefore, no associations found are statistically significant.
Conclusion: Overall survival length was low (average of 2 years), this may be because we looked at those who were diagnosed in 2013 or later, as these were the only ones we had full data available for. To increase sample size, outcomes could be explored in those who are still alive and the temporal relationship between ACB and outcomes could also be explored. Despite the limitations of the study, an increased susceptibility to falls, fractures and neuropsychiatric complications was seen with a rising ACB.
References: [1]Simonson, W. (2016) Anticholinergic properties of medications. Geriatric Nursing, 37(4):302-303 [2]Salahudeen, MS., Nishtala, PS. (2016) Examination and Estimation of Anticholinergic Burden: Current Trends and Implications for Future Research. Drugs & Aging, 33(5):305-313 [3]The Science of Parkinson’s. Does the age of onset make a difference? Available at: https://scienceofparkinsons.com/tag/age-of-onset/. Accessed: 7/02/2019. [4]Crispo, JAG., Willis, AW., Thibault, DP., Fortin, Y., Hays, HD., et al. (2016) Associations between Anticholinergic Burden and Adverse Health Outcomes in Parkinson Disease. PLOS One. [5]Ageing brain care. Anticholinergic cognitive burden scale (2012 update). Available at: http://www.miltonkeynesccg.nhs.uk/resources/uploads/ACB_scale_-_legal_size.pdf. Accessed: 7/02/2019.
To cite this abstract in AMA style:
S. Taylor, E. Jones. Does Anticholinergic Burden Affect the Outcomes in Patients Diagnosed with Parkinson’s Disease? [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/does-anticholinergic-burden-affect-the-outcomes-in-patients-diagnosed-with-parkinsons-disease/. Accessed April 25, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/does-anticholinergic-burden-affect-the-outcomes-in-patients-diagnosed-with-parkinsons-disease/