Session Information
Date: Sunday, October 7, 2018
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: The current study proposed to build a prediction model of clinical severity from the combination of multiple diffusion tensor derived indices in patients with progressive supranuclear palsy.
Background: By the presence of the involvement of cortical syndromes, a more general neural network might be disturbed in the later stage. The hypothesis is that microenvironmental changes from multiple brain regions, as detected by diffusion MRI, could reflect the disease severity. The point in this study is, trying to build up a useful model to predict the clinical severity because the neuropsychology evaluation is subjective and time consuming.
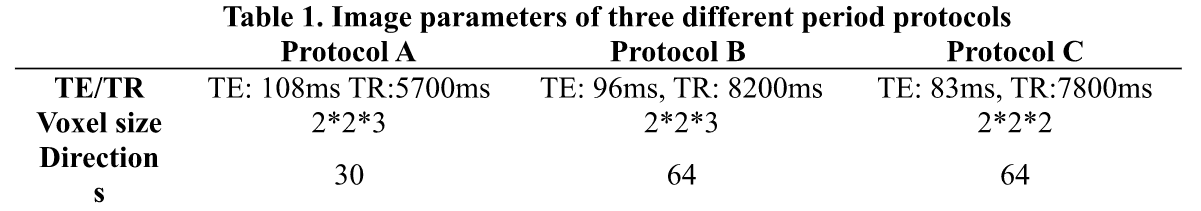
Methods: The current study was approved by International Review Board. Three different period protocols of diffusion tensor images were summarized in Table 1. Three protocols all included same contiguous 160 axial T1-weighted images acquired with magnetization-prepared rapid acquisition gradient echo sequence (T1-MPRAGE) (TE=2.63 ms, TR=2000 ms, flip angle= 9°, FOV=224mm×256mm, matrix size= 224×256, which leads to a voxel size=1mm x 1mm x 1mm, acquisition time= 4 min 08 sec) from a 3T MR scanner (MAGNETOM Trio a TIM system, Siemens, Germany). The diffusion images were parcellated into 246 brain regions according to the Brainnetome Atlas following Lu et al2. The 90th, 50th, and 10th percentile of the diffusion indices (Mean diffusivity and Fractional Anisotropy) were calculated. Clinical assessments including Unified Parkinson’s Disease Rating Scale (UPDRS), modified Hoehn and Yahr (mHY) were recorded. Spearman’s correlation was performed between diffusion indices in parcellated regions and the clinical assessments. Linear regression was performed using significant correlate brain regions to estimate the prediction variables. Two-tailed p value<0.01 was considered statistically significant.
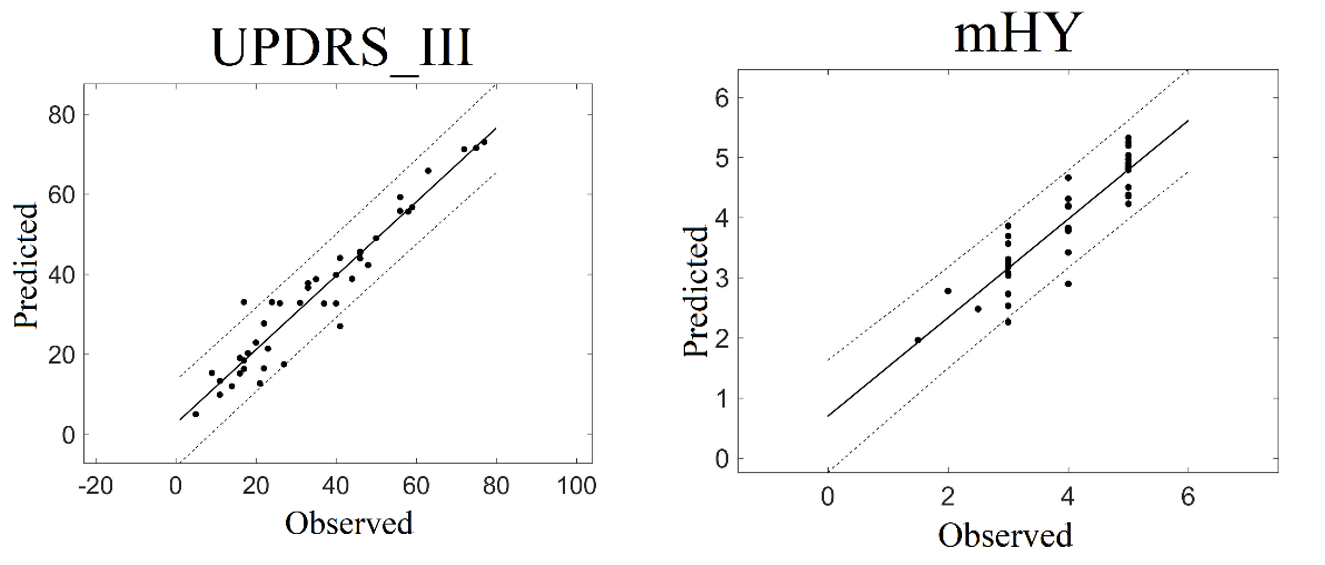
Results: Predicted clinical change for individual was listed in Table 2. The effect size (adjusted R2) of regression models was UPDRS_III (R2 = 0.92), mHY (R2 =0.82). The predicted and observed scores for the four models agree satisfactorily (Figure 1).
Conclusions: The clinical assessments in individuals with PSP can be accurately predicted by using diffusion tensor derived indices as measured from distinct brain regions.
References: 1. Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology, 1996; 47: 1-9. 2. Lu,C.S., Ng,S.H., Weng,Y.H., Cheng,J.S., Lin,W.Y., Wai,Y.Y., et al.(2016). Alterations of diffusion tensor MRI parameters in the brains of patients with Parkinson’s disease compared with normal brains: possible diagnostic use. Eur. Radiol. 26,3978–3988.doi:10.1007/s00330-016-4232-7.
To cite this abstract in AMA style:
X.A. Zhao, S.H. Lin, C.C. Tsai, Y.M. Wu, W.Y. Lin, Y.H. Weng, L.S. Lu, Y.L. Chen, J.J. Wang. Diffusion magnetic resonance imaging for predicting the severity of Progressive supranuclear palsy [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/diffusion-magnetic-resonance-imaging-for-predicting-the-severity-of-progressive-supranuclear-palsy/. Accessed December 22, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/diffusion-magnetic-resonance-imaging-for-predicting-the-severity-of-progressive-supranuclear-palsy/