Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: To assess the daily variability of visual and autonomic nervous system (ANS) functions in relation to sleep disorders to determine circadian PD phenotypes
Background: Many motor and non-motor manifestations of Parkinson disease (PD) exhibit diurnal oscillations. An abnormal retinal dopaminergic function and melanopsin-expressing Retinal Ganglion Cells (mRGC) degeneration leads to «melatonin-dopamine» imbalance and distortion of information transmitted through the retino-hypothalamic tract. This is one of the important factors of diurnal fluctuations of visual and autonomic dysfunction, sleep–wakefulness cycle disorders, etc. in PD.
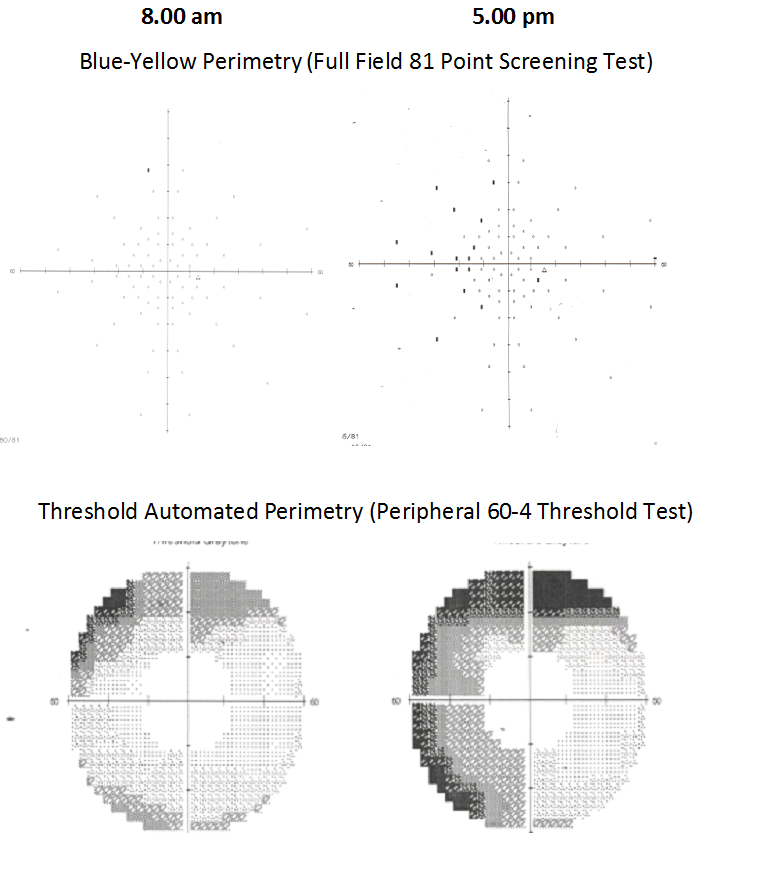
Method: 35 PD patients with 1–2.5 stages without motor fluctuations and 20 controls were examined at 8.00 am and 5.00 pm. Contrast sensitivity (CS), visual fields (VF) using threshold and Blue-Yellow perimetry (BYP), polysomnography, holter monitoring (HM) with determination of circadian index (CI) and sympathetic skin response (SSR) were investigated.
Results: In 21 patients (60%), daily variability of VF in the peripheral nasal segment and in the CS level, mostly for blue, was observed. A distinctive feature of these patients was a significant CI decrease according to HM, compared with PD patients without CS and VF daily variability. The most pronounced VF fluctuations with the appearance of widespread VF defects according to BYP at 5.00pm were noted in PD patients with visual hallucinations and REM-Behavior disorder [figure1]. Different nocturnal problems and daytime sleepiness were more pronounced and occurred more often in patients with VF and CS variability. SSR date revealed a predominance of parasympathetic effects on the sweat glands in most PD patients. In 24 PD patients (68.5%) who did not have daily variability of the SSR parameters, a significant CI reduction was detected, compared with healthy individuals and PD patients, in which the SSR parameters underwent changes between the morning and evening measurements.
Conclusion: Maximum sensitivity of mRGC to blue perception, the processing system of which is most vulnerable to circadian disorders, explains the features of the daily variability of CS and VF defects in PD. Changes in the properties of the retina in some PD patients make a significant contribution to circadian disorders of physiological processes and indicate the presence of different circadian PD phenotypes.
To cite this abstract in AMA style:
O. Alenikova, S. Likhchev, A. Buniak, M. Liashkovich. Daily variability of non-motor symptoms as a reflection of circadian dysregulation in Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/daily-variability-of-non-motor-symptoms-as-a-reflection-of-circadian-dysregulation-in-parkinsons-disease/. Accessed December 29, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/daily-variability-of-non-motor-symptoms-as-a-reflection-of-circadian-dysregulation-in-parkinsons-disease/