Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To assess psychological stress, through subjective and objective measures, in Parkinson’s disease (PD) prior to and during the worldwide pandemic.
Background: We have had an interest on the effect of psychological stress on PD. In human studies stress has been shown to worsen PD symptoms, including bradykinesia, freezing, and tremor [1,2,3]. Animal studies suggest that stress may have profound effects on the brain contributing to neuronal atrophy, reducing synaptic density, decreasing neurotrophic factors, worsening oxidative stress, and increasing the activity of the hypothalamic pituitary adrenal (HPA) axis [4]. We previously conducted a study looking at objective measures of stress and salivary cortisol in PD prior to the pandemic.
Method: Enrolled PD participants that lived within driving distance to Portland, Oregon were sent a letter offering re-enrollment, at home collection, and a short virtual visit. Participants were consented over the phone, collected their saliva 4 times a day for 3 days, completed a stress scale and a virtual visit. Samples were picked up from the participant’s houses within the week. All salivary samples were frozen.
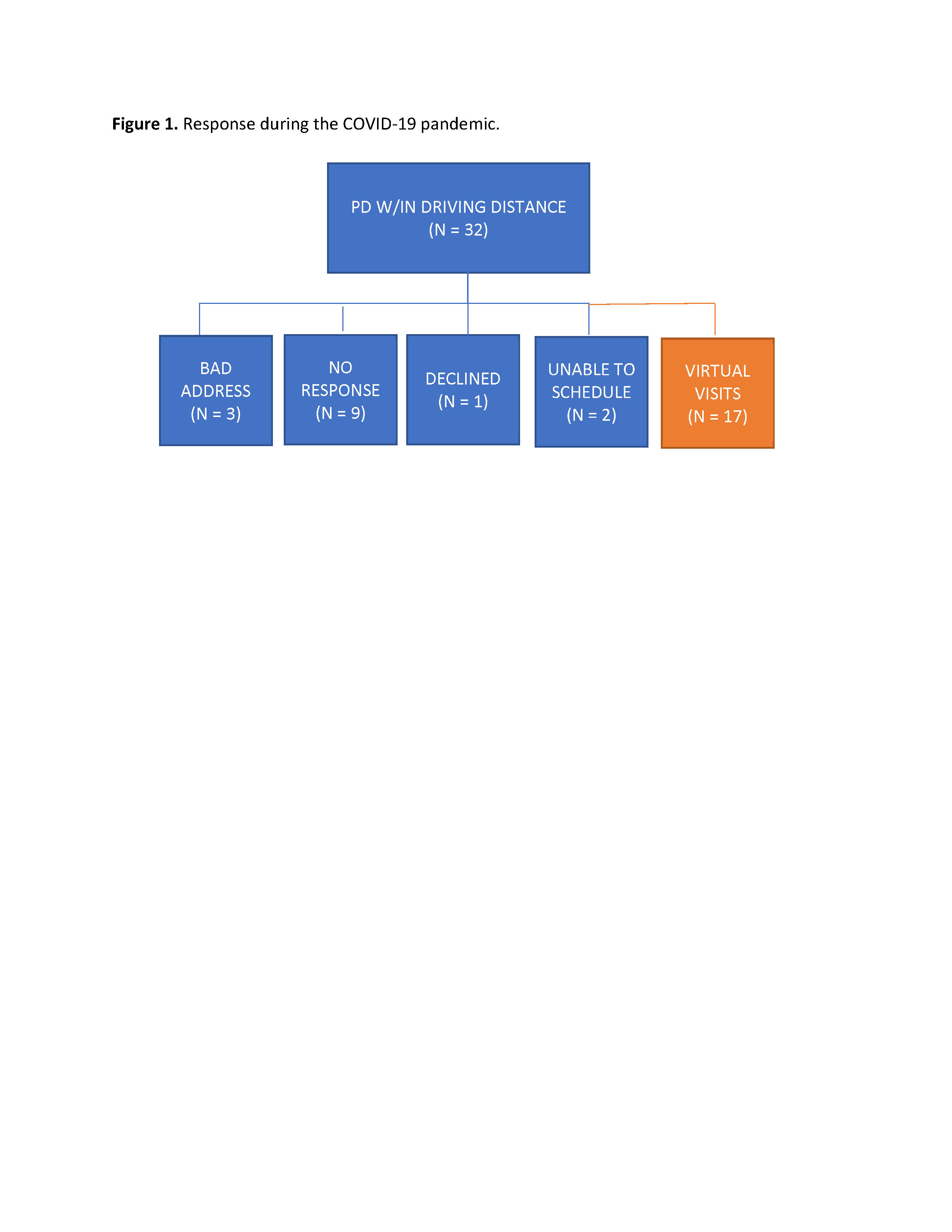
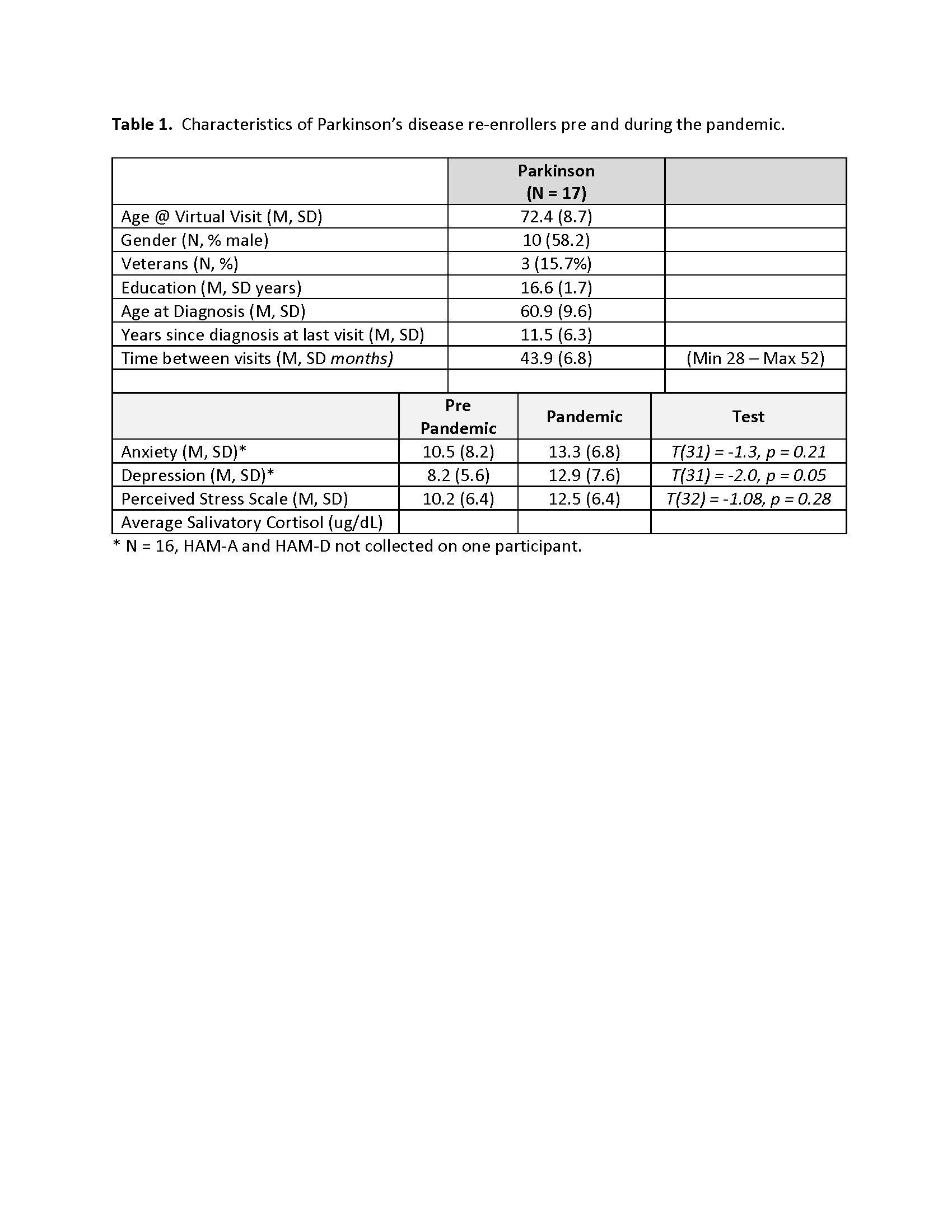
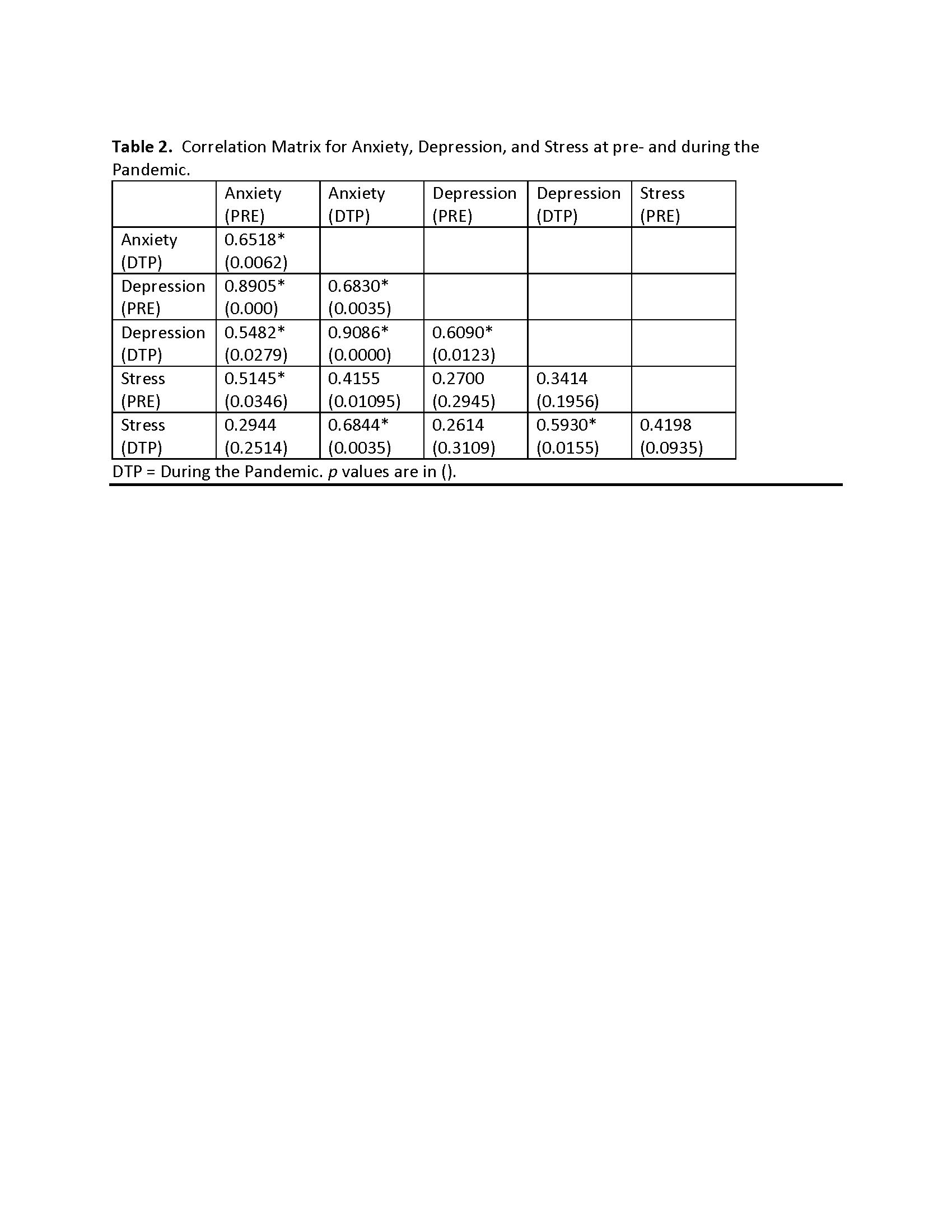
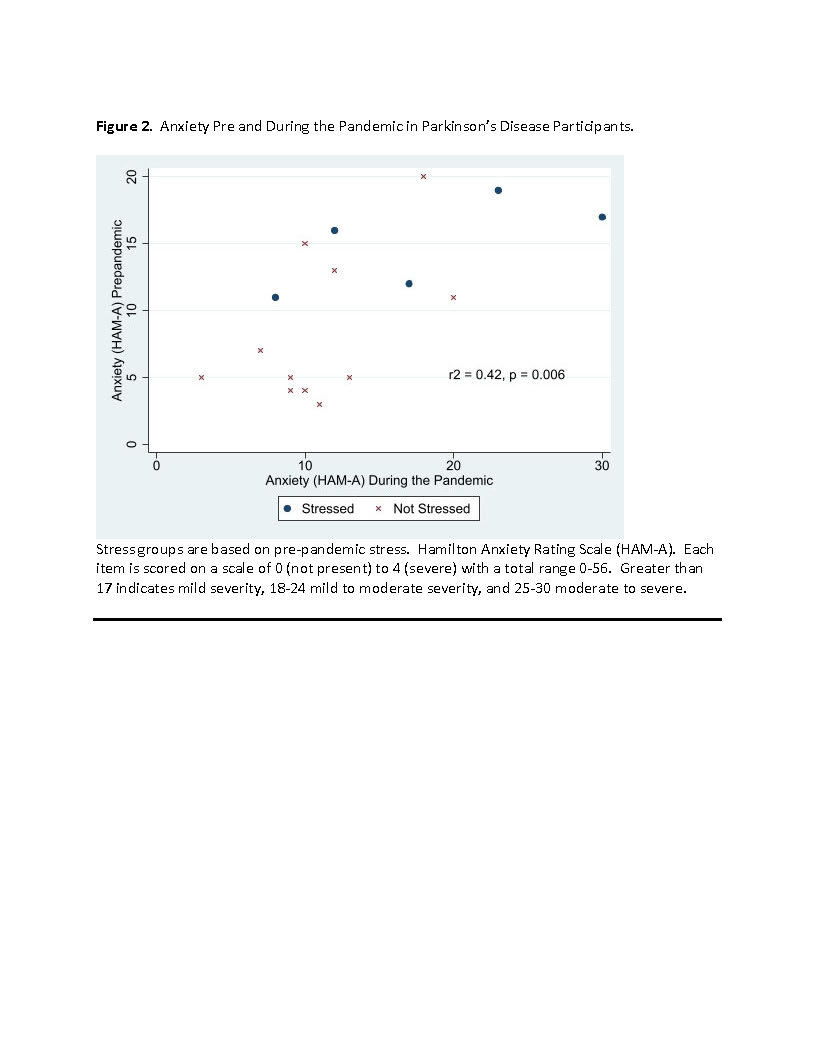
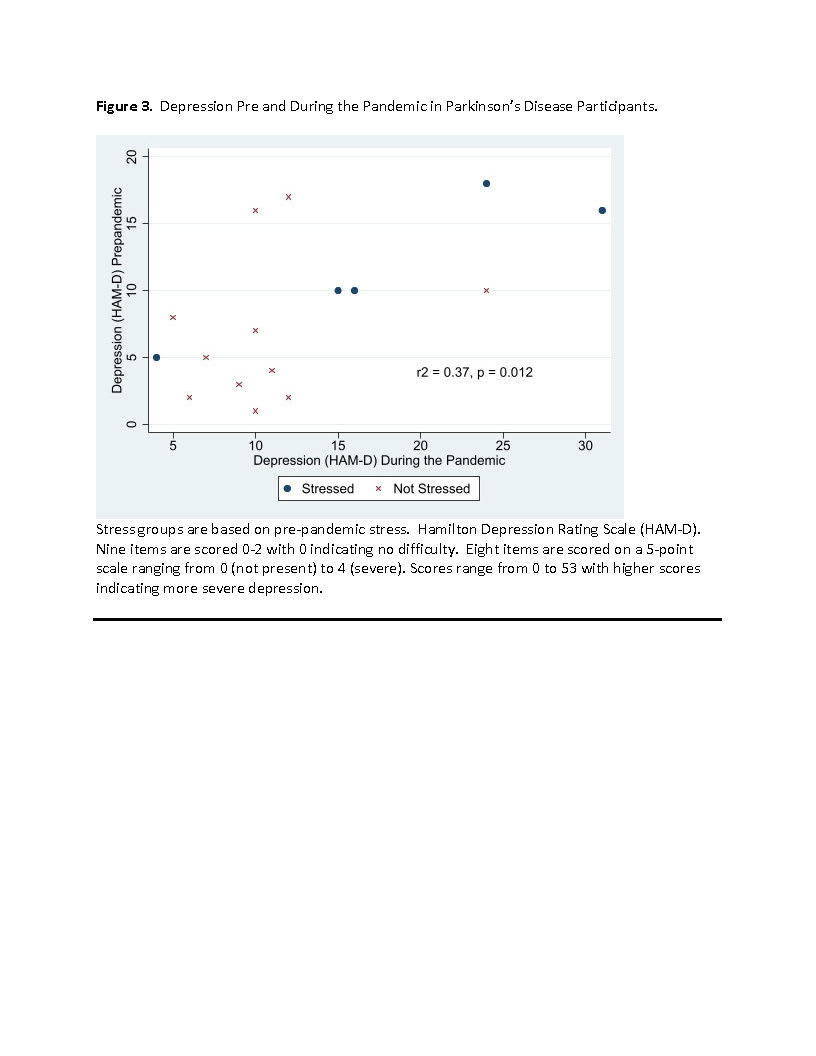
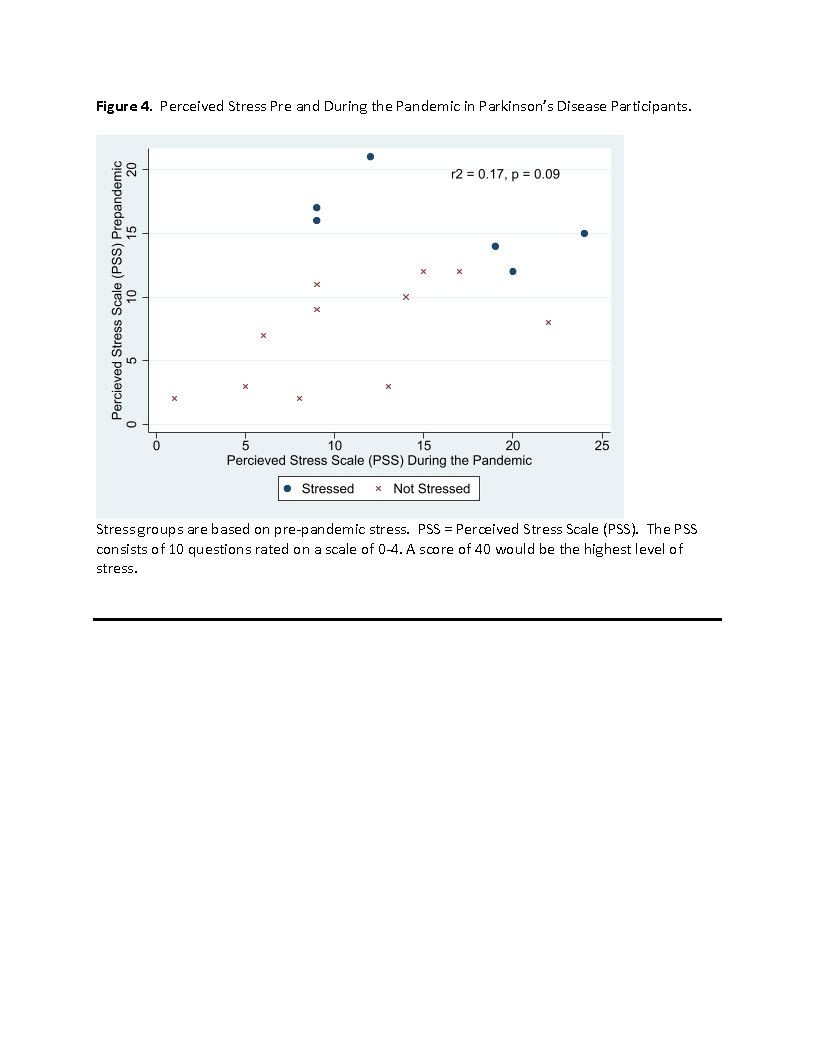
Results: Of the 32 potential re-enrollers, 9 did not respond, 1 declined, 3 had bad addresses, and 19 (66%) expressed interest. 17 virtual visits were completed (See Figure 1). Demographics of the sample are found in Table 1. For those that were stressed at the initial visit (N = 6), half (N = 3) were still stressed during the pandemic (DTP) visit. For those that were not stressed at the initial visit (N = 11), 5 were stressed DTP (45%). Anxiety (r = 0.65, p =0.006) and depression (r = 0.61, p = 0.012) were correlated pre and DTP (See Table 2/Figures 2-4). Perceived stress DTP was not highly correlated with pre pandemic stress (r = 0.42, p = 0.09). Salivatory cortisol will be analyzed and included in the future.
Conclusion: Surprisingly stress prevalence in this sample of PD from the Northwest was slightly lower than reports of the first seven months of the pandemic with only 47% reporting moderate to high stress. Depression and anxiety were persistent over time. The pandemic was not related to higher reports of perceived stress in this sample of PD but we only were able to re-enroll about two thirds or participants. It is possible that those with lower levels of stress were willing to participate and this may confound our results.
References: 1Smith, A.Castro, S. L. & Zigmond, M. J. (2002). Stress-induced Parkinson’s disease: a working hypothesis. Physiol. Behav. 77, 527-531.
2Marsden, C. D. & Owen, D. A. (1967). Mechanisms underlying emotional variation in parkinsonian tremor. Neurology 17, 711-715.
3Schwab, R. S. & Zieper, I. (1965). Effects of mood, motivation, stress and alertness on the performance in Parkinson’s disease. Psychiatr. Neurol. (Basel) 150, 345-357.
4Hemmerle, A. M., Herman, J. P. & Seroogy, K. B. (2012). Stress, depression and Parkinson’s disease. Exp. Neurol. 233, 79-86.
To cite this abstract in AMA style:
B. Lobb, A. Hiller. COVID-19 impact on Anxiety, Depression, Stress, and Cortisol in Persons with Parkinson’s Disease [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/covid-19-impact-on-anxiety-depression-stress-and-cortisol-in-persons-with-parkinsons-disease/. Accessed April 18, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/covid-19-impact-on-anxiety-depression-stress-and-cortisol-in-persons-with-parkinsons-disease/