Category: Ataxia
Objective: To describe a unique case of anti-metabotropic glutamate receptor 1 (mGluR1) antibody (Ab)-mediated cerebellar ataxia post-COVID-19 encephalitis.
Background: Cerebellar syndrome is increasingly recognised in COVID-19 infection [1]. Recent evidence implicates anti-glial fibrillary acidic protein Ab in post-COVID-19 cerebellar disease, suggesting an immunological aetiology [2]. Similarly, anti-mGluR1 Ab, with known propensity for cerebellar tissue, associates with autoimmune cerebellar syndrome, often with occult malignancy [3].
Method: Case report and literature review.
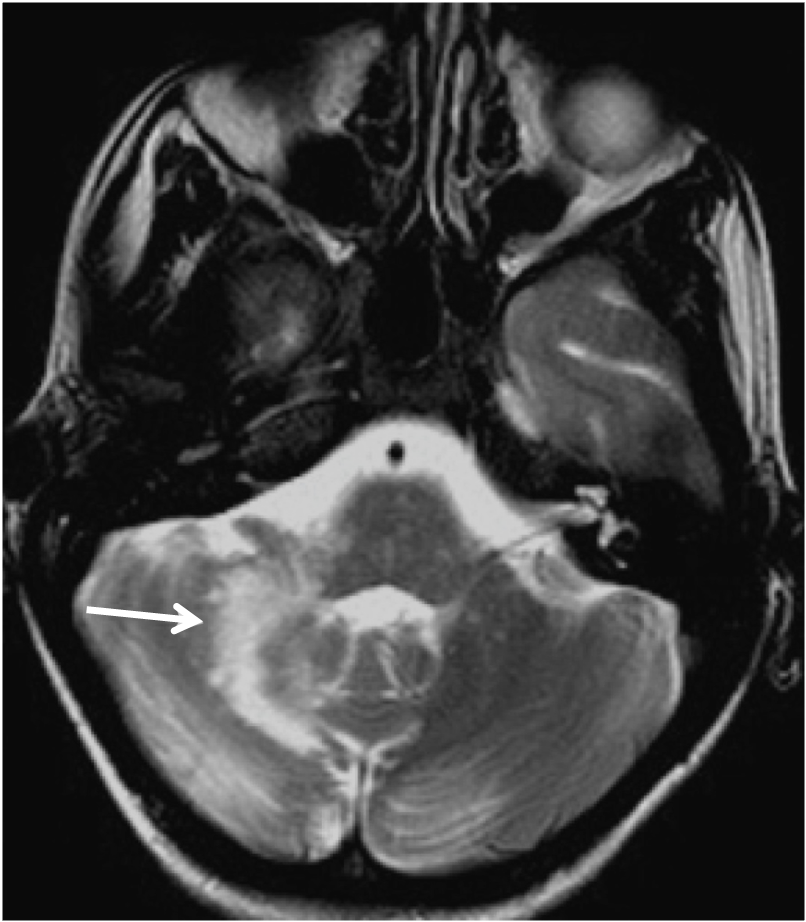
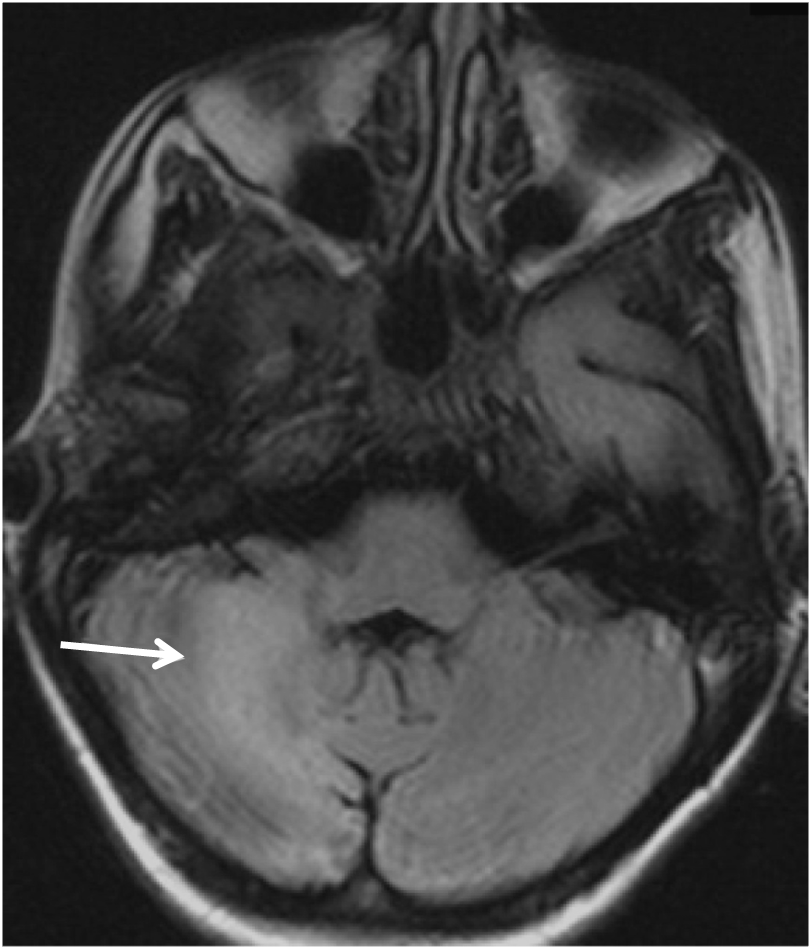
Results: A woman, 67, was admitted with breathlessness, headache, fever, confusion and positive SARS-CoV-2 nasal PCR. MRI brain showed non-specific white matter changes. Cerebrospinal fluid (CSF) showed leukocyte 23/mm^3, protein 1.4g/dL, glucose 2.9mmol/L and positive SARS-CoV-2 PCR. COVID-19 encephalitis was diagnosed. She improved with aciclovir and dexamethasone. 4 weeks post-hospital discharge, she re-presented with 10 days of imbalance, frequent falls and dysarthria, with no relevant family history. Examination revealed bilateral postural and intention hand tremors, asymmetric dysmetria and dysdiadochokinesis worse on the right, jerky saccades, broad-based ataxic gait, inability to tandem walk, upper limb myoclonus and global hyporeflexia. Repeat MRI showed new non-enhancing cerebellar white matter hyperintensities [Figure 1]. Repeat CSF showed leukocyte 69/mm^3 (80% lymphocytes), protein 1.9g/dL, glucose 2.6mmol/L and negative SARS-CoV-2 PCR. Serum and CSF anti-mGluR1 Ab were positive (1:1000 and 1:64). Extensive investigations including further serum and CSF autoimmune and paraneoplastic neuronal Abs, connective tissue Abs, copper and caeruloplasmin, blood film, infective and metabolic screens, and whole genome genetic testing for ataxia were negative or unremarkable. PET excluded malignancy. Sequential treatment with intravenous methylprednisolone, plasma exchange and mycophenolate mofetil ameliorated ataxia and myoclonus over 5 weeks and maintained remission at 12 months.
Conclusion: We identify the first case of COVID-19 encephalitis preceding immunotherapy-responsive anti-mGluR1 cerebellar syndrome. We postulate cerebral entry of SARS-CoV-2 immunologically precipitated subsequent anti-mGluR1 disease, expanding the spectrum of neurological COVID-19 manifestations and suggesting a novel pathogenic mechanism for COVID-19-induced cerebellar dysfunction.
References: 1. Dijkstra, F, Van den Bossche, T, Willekens, B, et al. Myoclonus and cerebellar ataxia following Coronavirus Disease 2019 (COVID-19). Movement Disorders Clinical Practice 2020; 7: 974–976.
2. Asan L, Klebe S, Kleinschnitz C, et al. Anti-GFAP-antibody positive postinfectious acute cerebellar ataxia and myoclonus after COVID-19: a case report. Therapeutic Advances in Neurological Disorders 2021; 14.
3. Spatola M, Pedrol MP, Maudes E, et al. Clinical features, prognostic factors, and antibody effects in anti-mGluR1 encephalitis. Neurology 2020; 95 (22).
To cite this abstract in AMA style:
F. Cheng, K. Tang, X. Wang. COVID-19 encephalitis with anti-mGluR1 antibody-positive cerebellar ataxia [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/covid-19-encephalitis-with-anti-mglur1-antibody-positive-cerebellar-ataxia/. Accessed January 28, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/covid-19-encephalitis-with-anti-mglur1-antibody-positive-cerebellar-ataxia/