Category: Parkinson's Disease: Pathophysiology
Objective: This study evaluated the correlation between neurofilament light chain (NfL) and freezing of gait (FOG) in Parkinson’s disease (PD).
Background: PD patients frequently experience FOG. The mechanisms of FOG remain unclear and lacks effective biological predictors.
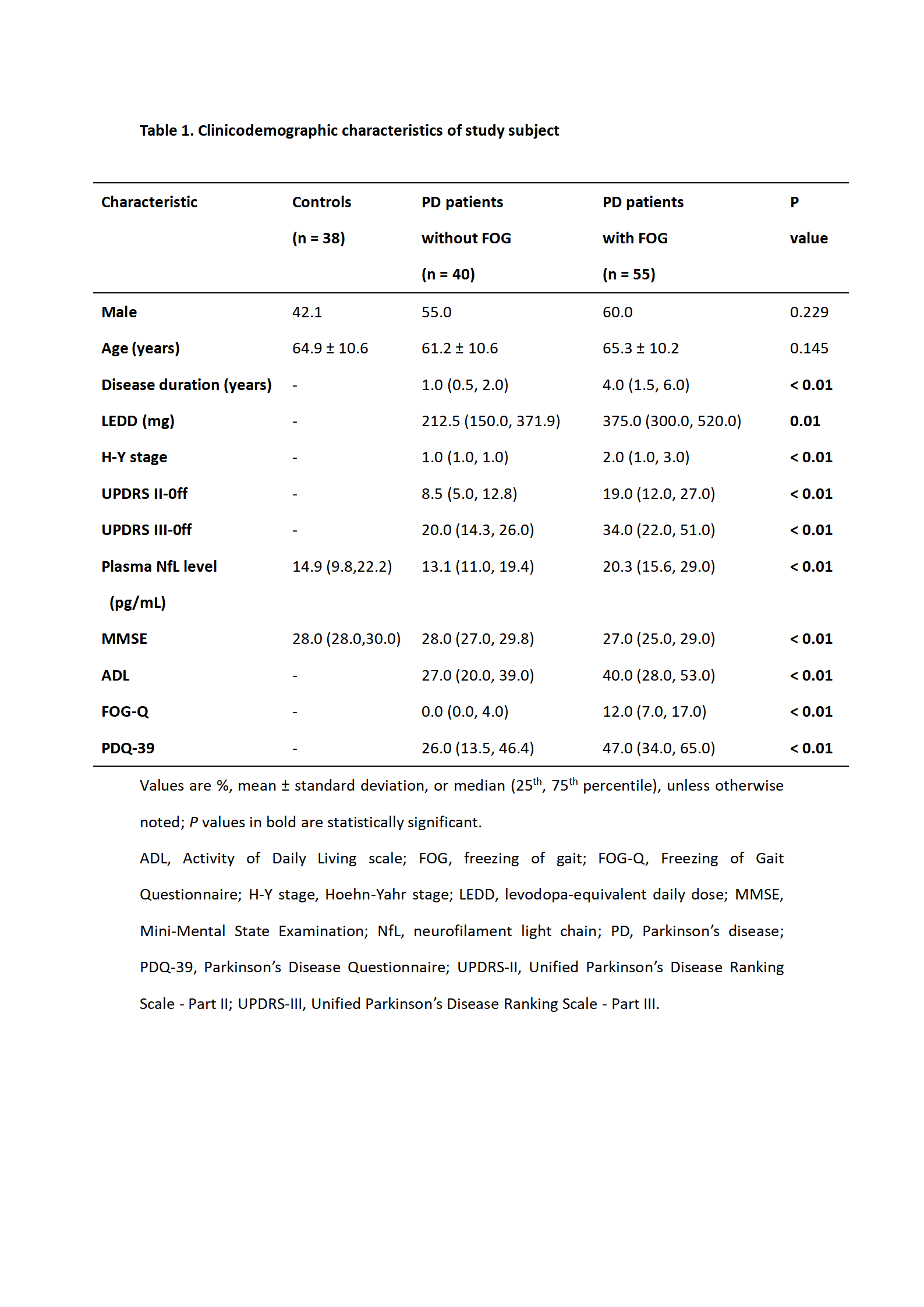
Method: This study recruited 95 PD patients (55 with FOG and 45 without FOG) and 38 healthy controls from the First Affiliated Hospital of Kunming Medical University. The FOG Questionnaire (FOG-Q)[3]was used to stratify PD patients into two groups depending on whether they experienced FOG or not. We compared plasma NfL among patients with or without FOG as well as controls. Receiver operating characteristic (ROC) curve analysis was used to determine the threshold value of NfL required to distinguish patients with or without FOG.Binary logistic regression was used to identify risk factors associated with FOG in PD patients.
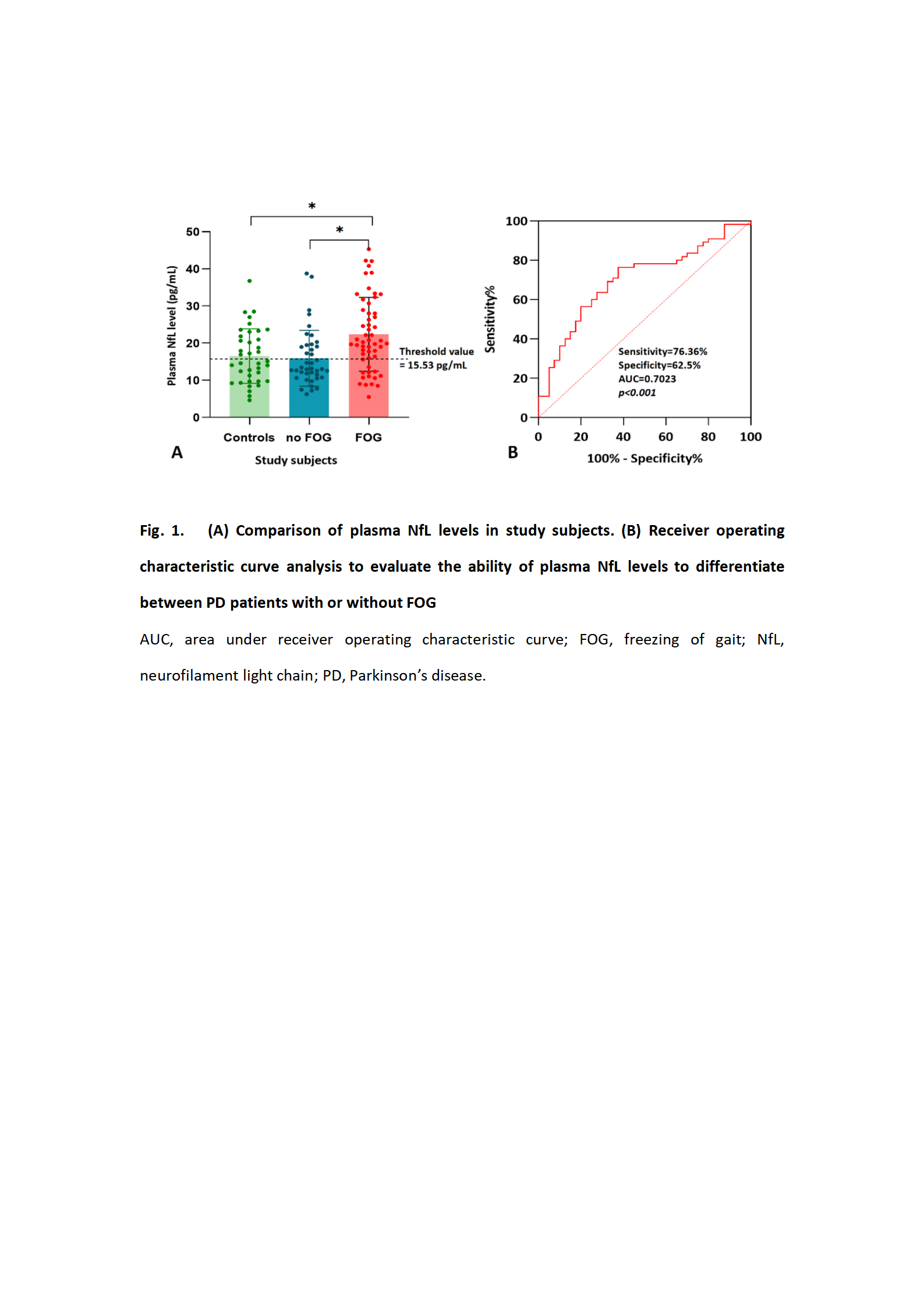
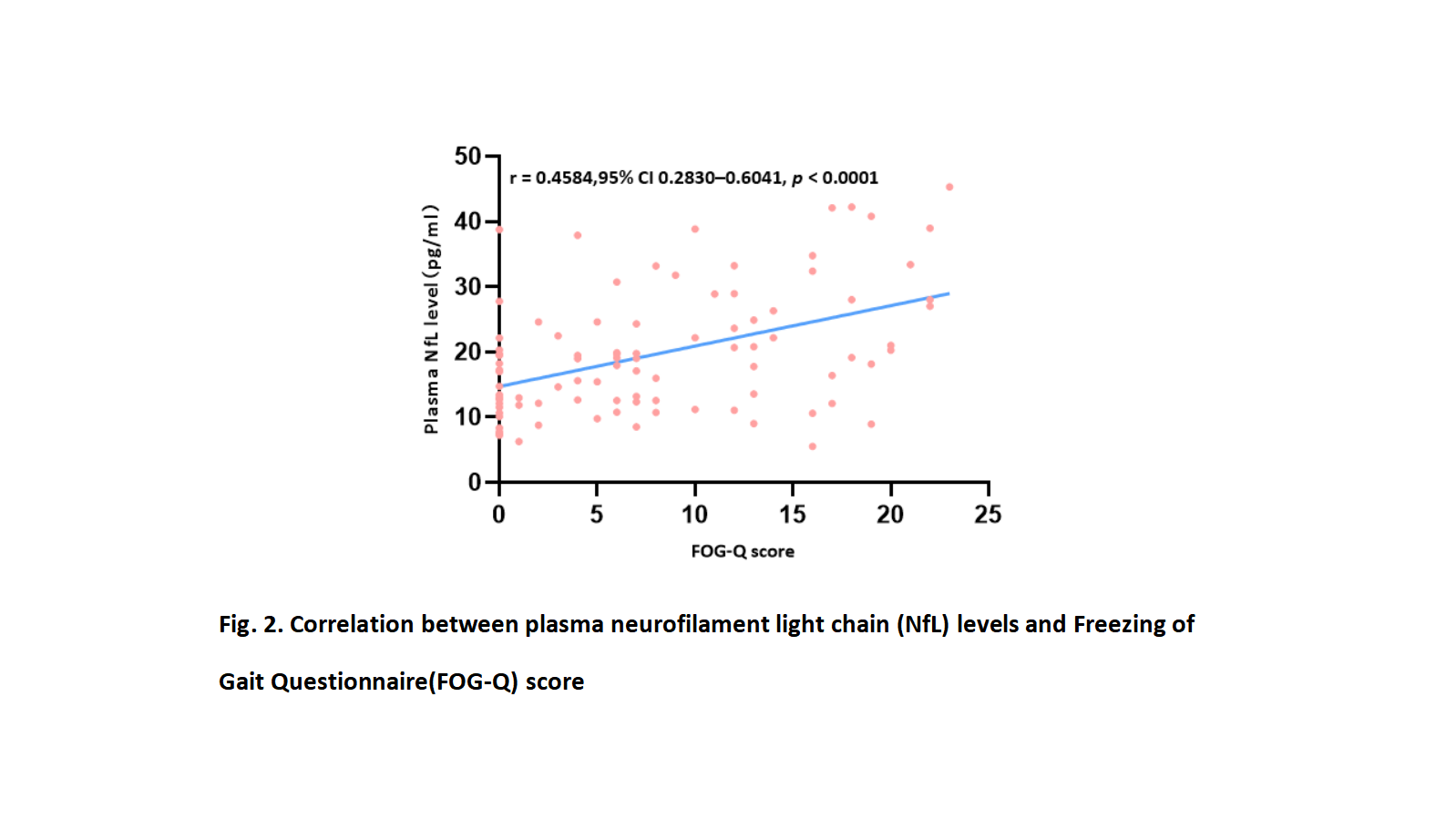
Results: PD patients with FOG had significantly higher plasma NfL (20.3 (15.6, 29.0)) than controls (14.9 (9.6, 22.2) and patients without FOG (13.1 (11.0, 19.4)(shown in Table 1, Fig. 1A). Plasma NfL positively correlated with FOG-Q score in PD (r= 0.4584,95% CI 0.2830–0.6041, p < 0.0001,shown in Fig.2). Based on the ROC analysis, we found that a plasma NfL level of 15.53 pg/mL was able to differentiate between PD with or without FOG, corresponding to a sensitivity of 76.36%, specificity of 62.50%, and area under the curve of 0.7023 (shown in Fig. 1A-B).
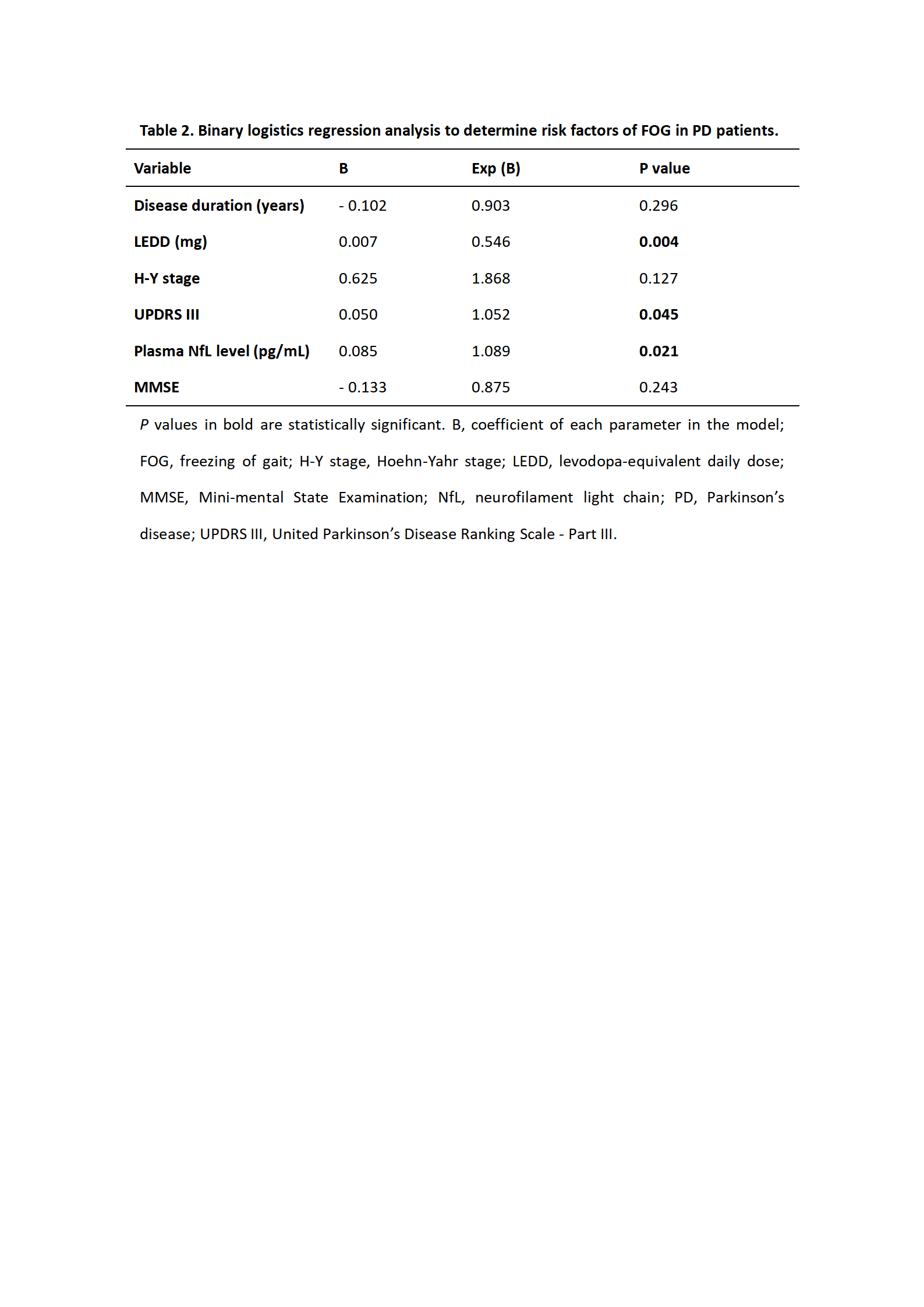
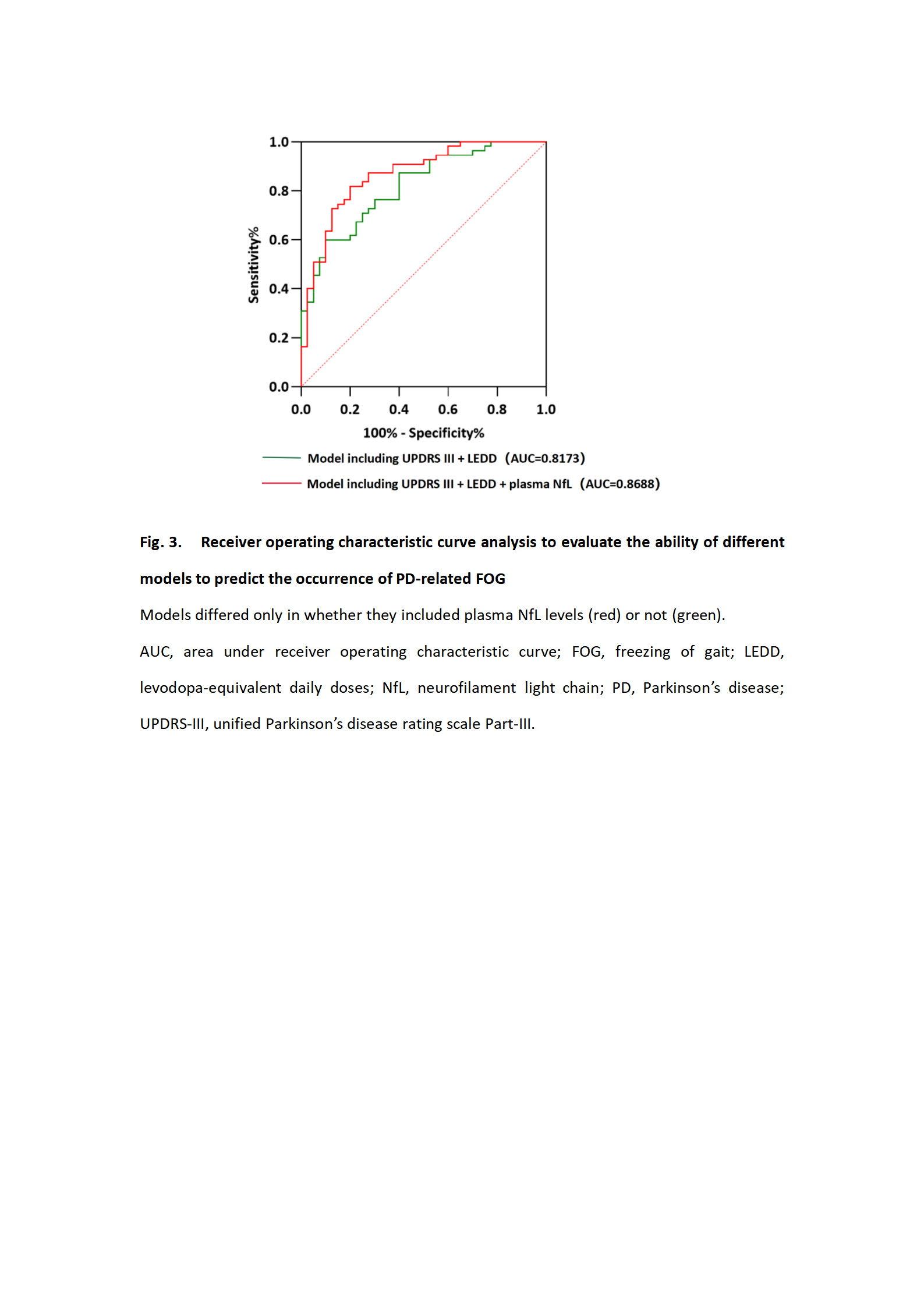
Binary logistic regression identified levodopa-equivalent daily doses (LEDD), the Unified Parkinson Disease Rating Scale-Part III (UPDRS III), and NfL as independent risk factors of FOG in PD (Table 2). Based on ROC curves, we found that the model with all three variables (LEDD + UPDRS III + NfL) showed higher prediction accuracy (AUC = 0.8668, 95% confidence interval (CI) 0.7935-0.9401, P < 0.0001) than the model that omitted NfL (AUC 0.8173, 95% CI 0.7342-0.9003, P < 0.0001; shown in Fig. 3).
Conclusion: Our results indicate that high plasma NfL may be useful for differentiating between PD who experience FOG and those who do not. Importantly, we also found that a combination of plasma NfL, UPDRS III scores and LEDD can increase the prediction accuracy of FOG occurrence in PD.
References: [1] Giladi N, Nieuwboer A. Understanding and treating freezing of gait in parkinsonism, proposed working definition, and setting the stage [J]. Mov Disord, 2008, 23 Suppl 2(S423-5. 10.1002/mds.21927
[2] Khalil M, Teunissen C E, Otto M, et al. Neurofilaments as biomarkers in neurological disorders [J]. Nat Rev Neurol, 2018, 14(10): 577-89. 10.1038/s41582-018-0058-z
[3] Giladi N, Shabtai H, Simon E S, et al. Construction of freezing of gait questionnaire for patients with Parkinsonism [J]. Parkinsonism Relat Disord, 2000, 6(3): 165-70. 10.1016/s1353-8020(99)00062-0
To cite this abstract in AMA style:
Y. Zhu, X. Yang, H. Ren, A. Pang. Correlation between levels of plasma neurofilament light chain and freezing of gait in Parkinson’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/correlation-between-levels-of-plasma-neurofilament-light-chain-and-freezing-of-gait-in-parkinsons-disease/. Accessed December 30, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/correlation-between-levels-of-plasma-neurofilament-light-chain-and-freezing-of-gait-in-parkinsons-disease/