Category: Technology
Objective: To develop a contactless assessment model for rigidity evaluation in Parkinson’s Disease (PD)
Background: Rigidity in PD is evaluated manually in current practice, and examiners need to touch the patient, move the limbs and score the severity of symptoms by feeling muscle tone abnormalities; thus, contact was a prerequisite. A contactless evaluation system for rigidity has never been explored. Our research aims to develop a rigidity rating system without contact by machine vision and machine learning.
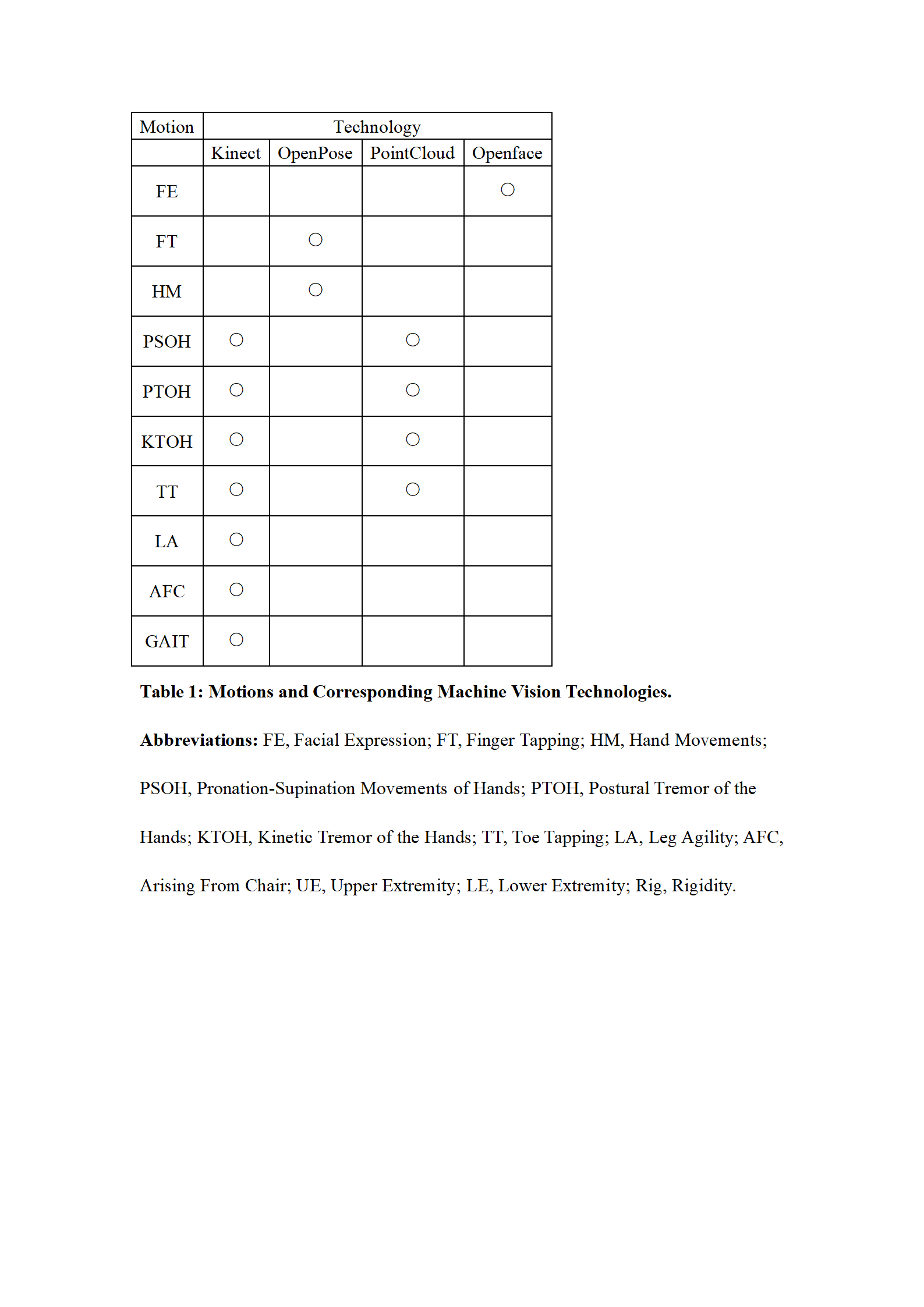
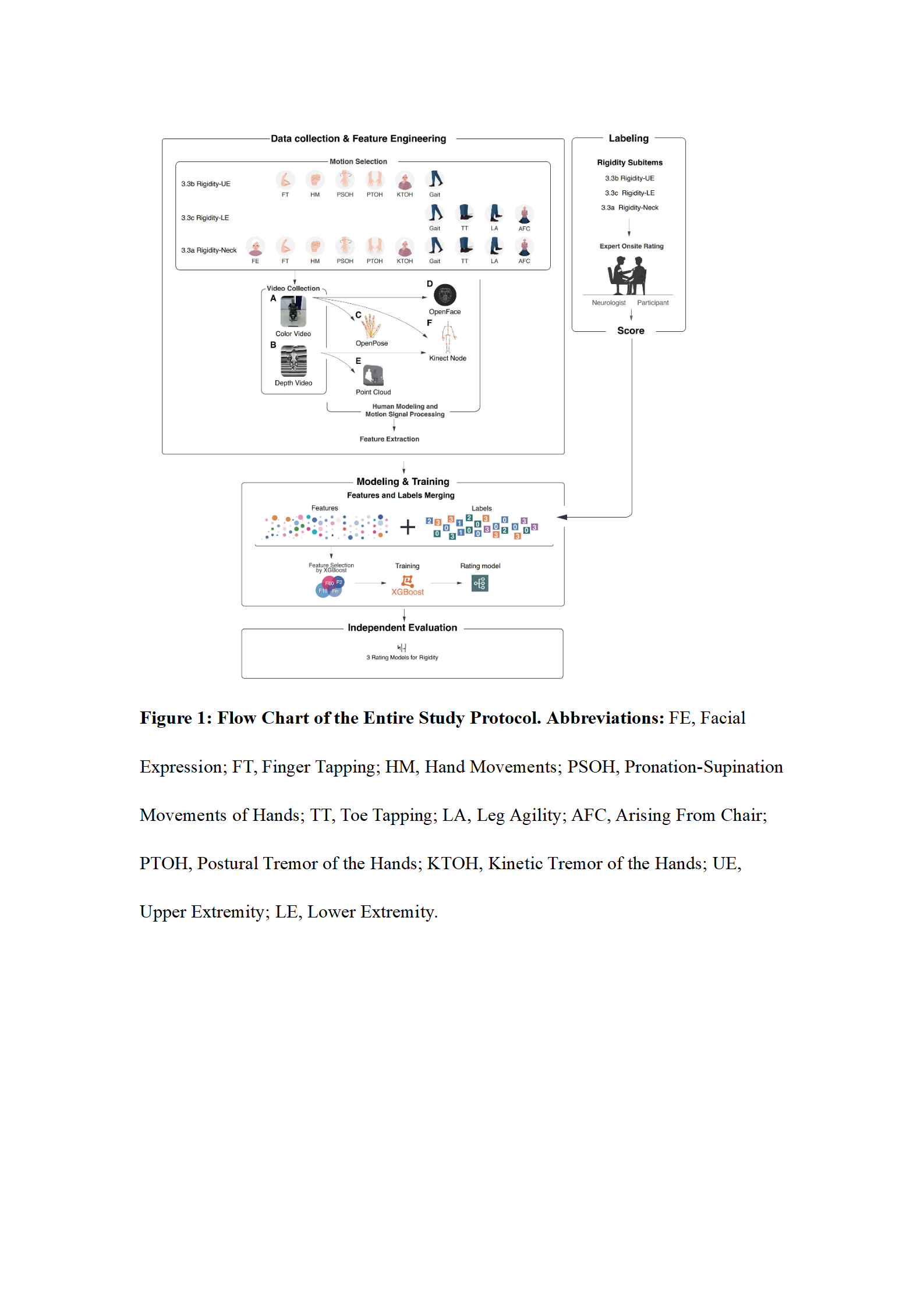
Method: Machine vision technologies were integrated to extract features from videos of active motions (112 patients) based on the MDS-UPDRS III instructions [Table 1]. Extreme Gradient Boosting (XGBoost) conducted feature selection and model training with the extracted features and rigidity rating from expert rater [Figure 1]. An independent test (23 patients) was used for validation. Consistency (intraclass correlation coefficient, ICC), correlation (Spearman correlation coefficient, ρ) and absolute accuracy (ACC±0) between model and expert rating were calculated as model performance. Features selected by XGBoost encompassed four dimensions: motion, joint, signal, and attribute.
Results: In the model of Rigidity-Upper Extremity, consistency and correlation were moderate (ICC=0.60, ρ=0.64) and ACC±0 was 0.65. In the model of Rigidity-Lower Extremity, consistency and correlation were moderate (ICC=0.60, ρ=0.58), and ACC±0 was 0.72. For Rigidity-Neck, consistency and correlation were also moderate (ICC=0.70, ρ=0.67), and ACC±0 was 0.78 [Table 2].
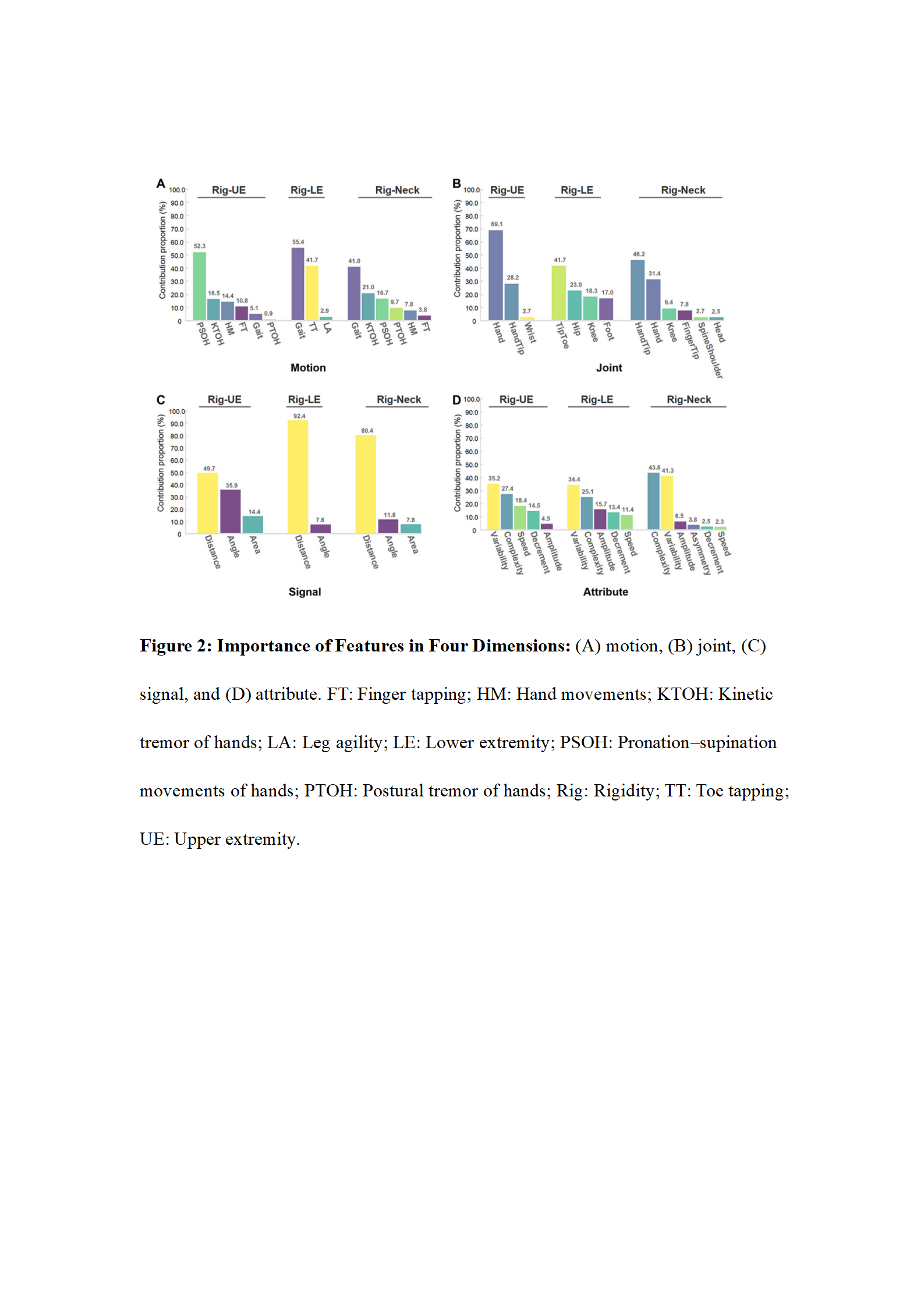
In terms of motion, Gait contributed the most in 2 models. In terms of joints, features from distal positions had greater importance. Regarding signals, distance contributed the most. The large radius of motion captured by the distal portion of the body carried movement signals representing the rigidity of the proximal joint. For example, the motion of the hand pointing to and away from the nose served as a proxy for elbow rigidity. As to attributes, complexity and variability were the 2 main contributors in all models [Figure 1]. Conversely, features described in the MDS-UPDRS III scale, such as speed, amplitude, decrement and asymmetry, contributed less. Machine vision captured more information than those observed by human raters.
Conclusion: Contactless rigidity evaluation in PD is feasible and may facilitate remote care for PD patients by telemedicine in the future.
To cite this abstract in AMA style:
X. Zhu, W. Shi, Y. Ling, N. Luo, Q. Yin, Y. Zhang, A. Zhao, G. Ye, H. Zhou, J. Pan, L. Zhou, L. Cao, P. Huang, P. Zhang, Z. Chen, C. Chen, S. Lin, J. Zhao, K. Ren, Y. Tan, J. Liu. Contactless assessment of rigidity in Parkinson’s disease using machine vision and machine learning [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/contactless-assessment-of-rigidity-in-parkinsons-disease-using-machine-vision-and-machine-learning/. Accessed December 20, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/contactless-assessment-of-rigidity-in-parkinsons-disease-using-machine-vision-and-machine-learning/