Category: Surgical Therapy: Parkinson's Disease
Objective: To assess the relationship between deep brain stimulation (DBS)-induced improvements on motor symptoms and activities of daily living (ADL) in a single-center cohort of Parkinson’s disease (PD), dystonia and essential tremor (ET) patients.
Background: DBS is an established treatment for movement disorders including PD, dystonia and ET. A recurring question in assessing the effect of DBS is whether the changes on the motor scale with which the clinical effect is assessed correlates with an improvement in ADL. Since this is of crucial relevance for outcome evaluation and the management of expectations, we investigated this in a single-center DBS cohort.
Method: Motor and ADL outcome scores were obtained before and six to twelve months after surgery for 172 PD, 31 dystonia, and 21 ET patients. For motor assessment, in PD we used the Movement Disorders Society Unified Parkinson’s Disease Rating Scale Motor Examination (MDS UDPRS-III), for dystonia the Burke-Fahn-Marsden Dystonia Rating Scale motor score (BFMDRSms) and for ET the Essential Tremor Rating Scale (TETRASp). For ADL assessment, the MDS UPDRS ADL (MDS UPDRS-II) was used for PD, items of the AMC Linear Disability Scale (ALDS) for dystonia and the TETRAS-ADL for ET patients. In dystonia patients, the effect of presence of psychiatric history was further explored. For each cohort, changes in motor scores were correlated to changes in ADL scores using Spearman Rank correlation.
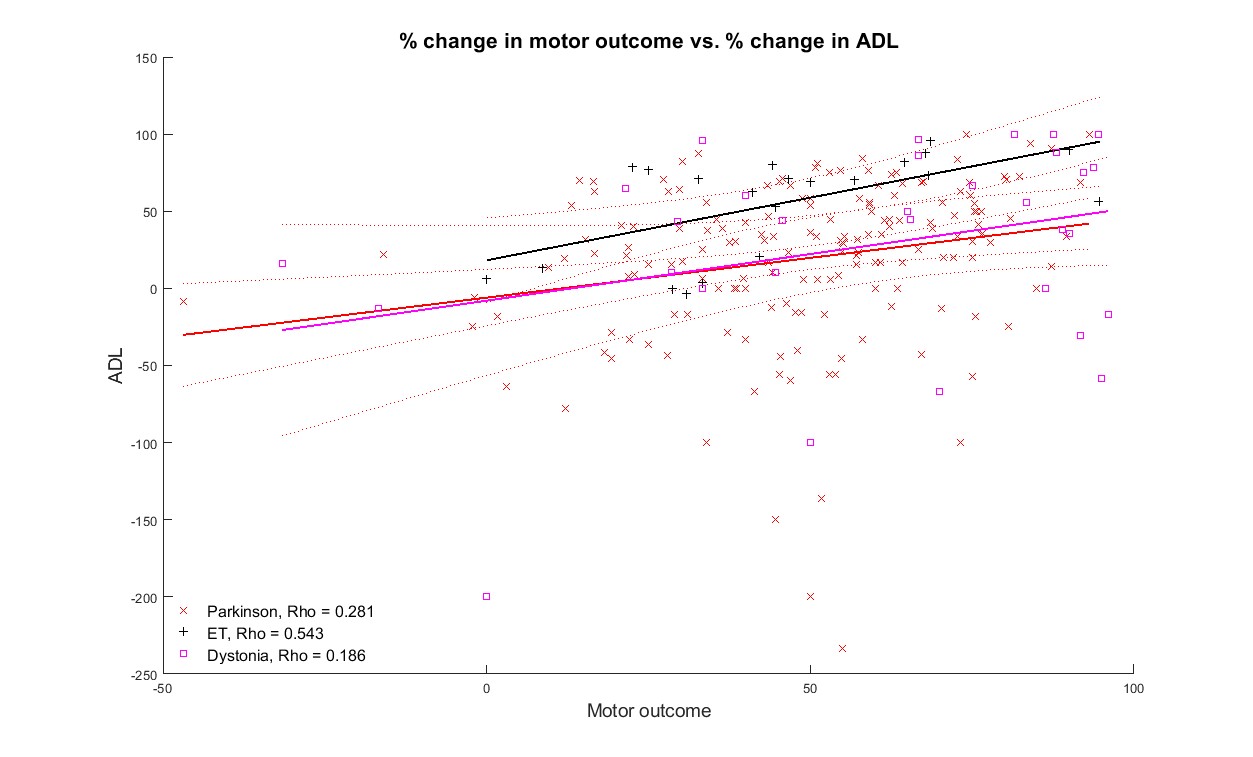
Results: For dystonia, there was a low correlation between motor and ADL improvement (Rho=0.186, p=0.317), while a modest and strong correlation were found for respectively PD and ET (Rho=0.281, p=0.001, Rho=0.543, p=0.011) (Figure 1). When dividing the dystonia group into a group with and without psychiatric symptoms, the correlation increased for the group without and decreased for the group with psychiatric symptoms.
Conclusion: The robust correlation between motor improvement and ADL in ET is concordant with the hypothesis that predominantly motor symptoms determine ADL. The modest and low correlations in PD and dystonia suggest that level of ADL in case of these diseases is also driven by non-motor symptoms. This is further illustrated by the fact that his correlation is even lower in patients with a psychiatric history. For dystonia, the degree of ADL change and low correlation is in line with other cohorts using different ADL scales1,2.
References: 1. Eggink H, Toonen RF, van Zijl JC, van Egmond ME, Bartels AL, Brandsma R, et al. The Effectiveness of Deep Brain Stimulation in Dystonia: A Patient-Centered Approach. Tremor Other Hyperkinet Mov (N Y). 2020;10:2.
2. Huebl J, Andermann T, Blahak C, Krauss J, Südmeyer M, Volkmann J, Bötzel K, Wolters A, Kühn A. Impact of pallidal deep brain stimulation on activites of daily living in patients with craniocervical dystonia – a multi-center survey. Int. Park. And Mov. Disorder Society Abstract. 2019.
To cite this abstract in AMA style:
Y. Wiggerts, E. Markidis, A. Weide, M. Bot, V. Odekerken, P. Munckhof, J. Dijk, Y. Namavar, R. Schuurman, R. Bie, M. Beudel. Comparing Change in Motor and ADL Rating Scales after DBS in Parkinson’s disease, Dystonia and Tremor [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/comparing-change-in-motor-and-adl-rating-scales-after-dbs-in-parkinsons-disease-dystonia-and-tremor/. Accessed December 22, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/comparing-change-in-motor-and-adl-rating-scales-after-dbs-in-parkinsons-disease-dystonia-and-tremor/