Objective: To identify clinical and objective gait measures that best discriminate fallers from non-fallers in Parkinson’s disease (PD), with suggestions of optimal cutoff scores
Background: The multifactorial nature of falls in PD is well described [1], [2]. Clinical aspects (e.g., fear of falling and disease severity) and gait deficits (e.g. difficulties with dual-task walking and freezing of gait episodes) are among identified risk factors of falling [1], [3]. However, optimal assessment for the identification of fallers remains unclear.
Method: Individuals with mild to moderate PD were classified as fallers (≥2 falls) or non-fallers based on previous 12 months falls. Clinical measures (demographic, motor, cognitive and patient-reported outcomes) were assessed with standard scales/tests. For measuring gait parameters, participants were asked to walk, at a self-selected pace, back and forth on a straight 9-m walkway for 2 minutes in single and dual-task (i.e., forward digit span) conditions, while instrumented with eight, synchronized inertial sensors at the sternum, lumbar spine, bilaterally on the wrists, shins, and feet.
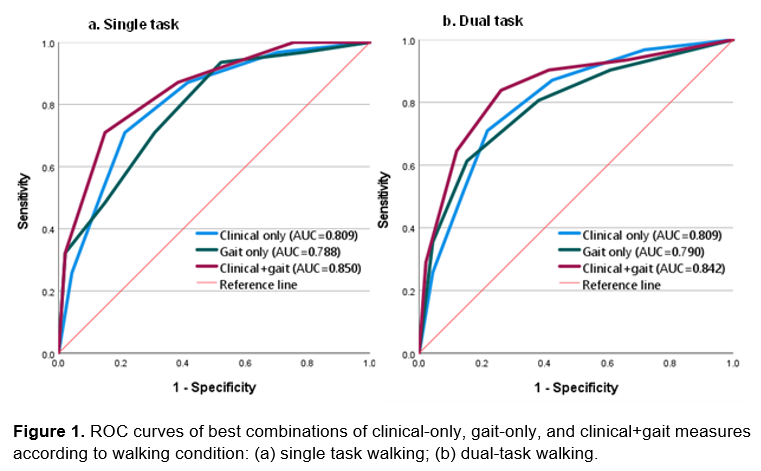
Receiver operating characteristic (ROC) curve analysis identified measures (separately and in combination) that best discriminate fallers from non-fallers; we calculated the area under the curve (AUC) and identified optimal cutoff scores (i.e., point closest-to-(0,1) corner).
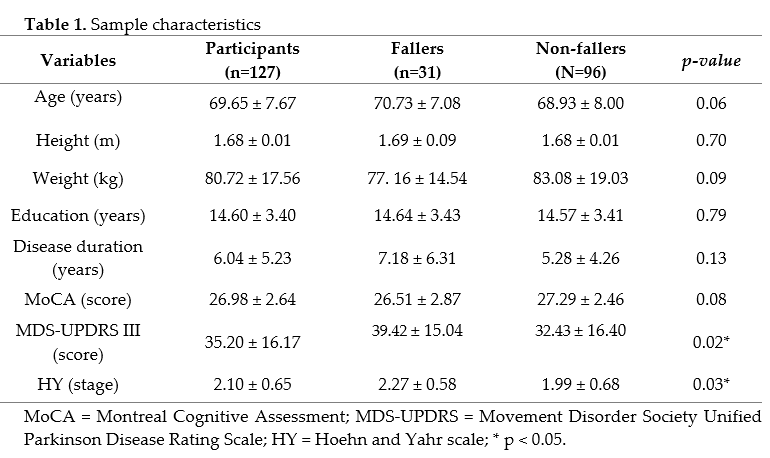
Results: Thirty-one participants (24.4%) were classified as fallers and 96 (75.6%) as non-fallers. Demographics and clinical characteristics are shown in Table 1. Fallers had more severe motor symptoms and more advanced disease stage than non-fallers (Table1).
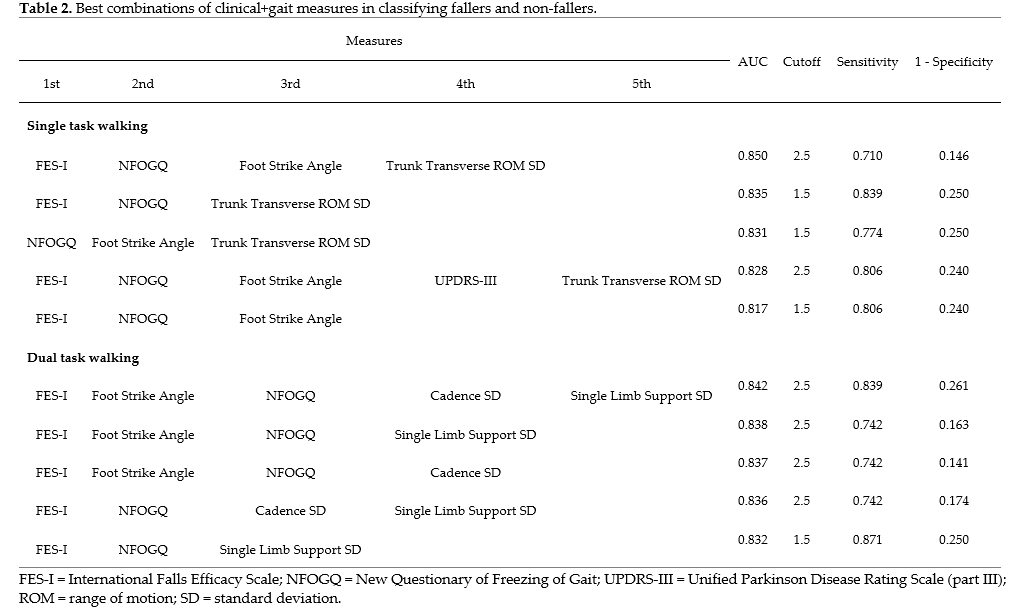
Single gait and clinical measures that best classified fallers were foot strike angle (AUC=0.728; cutoff=14.07°) and the Falls Efficacy Scale International (FES-I; AUC=0.716, cutoff=25.5), respectively. Combinations of clinical+gait measures had higher AUCs than combinations of clinical-only or gait-only measures (Figure 1). The best performing combination included FES-I score, New Freezing of Gait Questionnaire score, foot strike angle and trunk transverse range of motion (AUC=0.85) (Table 2).
Conclusion: The combinations of clinical and gait measures have higher discriminative ability in classifying fallers from non-fallers among people with PD than combinations of clinical-only and gait-only measures.
References: [1] N. E. Allen et al., “Interventions for preventing falls in Parkinson’s disease,” Cochrane Database Syst. Rev., vol. 2022, no. 6, 2022, doi: 10.1002/14651858.CD011574.pub2.
[2] S. S. Paul, L. E. Dibble, and D. S. Peterson, “Motor learning in people with Parkinson’s disease: Implications for fall prevention across the disease spectrum,” Gait Posture, vol. 61, no. December 2017, pp. 311–319, 2018, doi: 10.1016/j.gaitpost.2018.01.026.
[3] C. L. Owen, K. Ibrahim, L. Dennison, and H. C. Roberts, “Falls Self-Management Interventions for People with Parkinson’s Disease: A Systematic Review,” J. Parkinsons. Dis., vol. 9, no. 2, pp. 283–299, 2019, doi: 10.3233/JPD-181524.
To cite this abstract in AMA style:
H. Araújo, S. Smaili, J. Das, R. Morris, S. Stuart, R. Vitorio. Combination of clinical and gait measures to classify fallers and non-fallers in Parkinson’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/combination-of-clinical-and-gait-measures-to-classify-fallers-and-non-fallers-in-parkinsons-disease/. Accessed February 6, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/combination-of-clinical-and-gait-measures-to-classify-fallers-and-non-fallers-in-parkinsons-disease/