Objective: Describe a patient in which after starting continuous infusion of LECIG a large reduction of the LEDD is achieved.
Background: Gastroparesis (GP) is one of the non motor symptoms (NMS) of Parkinson’s disease (PD), might interfere with the absorption of drugs and have a significant impact on quality of life. Slower gastric emptying correlated with higher mean doses of Dopa Decarboxylase Inhibitor. Catechol-O-methyl transferase (COMT) inhibitors are associated with reduction in hypoactive GI symptoms. GP need a multidisciplinary approach. When all strategies are ineffective, an alternative approach is transition to non-oral therapies. Continuous intraduodenal infusion of LD/CD has proven to be an effective method to control motor and NMS in PD patients. It is recommended During the titration of LCGI a 20% reduction of the previous oral LEDD is implemented, increasing the reduction up to 33% after the infusion of LECIG begins.
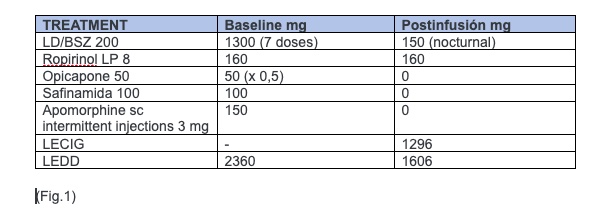
Method: A 75 yo woman with advanced PD, severe motor fluctuations with more than 6 hours a day in OFF state, mild ON dyskinesia and severe fluctuating NMS (digestive, anxiety), MDS UPDRS I=17, II= off 25, on 3, III= off 43, on 17, IV=13. Treated with 7 doses of LD/BSZ, IMAO, ICOMT, DA and apomorphine rescues. LEDD=2366. Treatment with LECIG was started, but as a severe problem of GP and malabsorption of LD was suspected, only 50% of the LEDD was calculated as the initial dose. Starting parameters were: morning dose 9 ml, continuous infusion 16 h/d 2,5 ml/h, extra dose (ED) 1.5 ml, oral medication was discontinued except DA (to avoid withdrawal syndrome) and nocturnal LD/BSZ dose.
Results: Optimization was performed with significant improvement in motor and NM symptoms. LEDD after PEG-J tube insertion was 1296 mg (55% reduction on infusion and 33% in total treatment). Further details in the patient’s treatment shown in fig1. Patient maintained an on state all day, mild dyskinesia only requiring 2 ED. Improvement of sleep, anxiety, constipation and abdominal pain. MDS UPDRS IV=7, PCG-I= 1 (very much better).
Conclusion: LECIG is a new available option in advanced PD patients. Our patient with severe GI dysmotility benefited from receiving this direct intraduodenal therapy, with no adverse effects, major improvement in her symptoms and an important reduction in total LEDD.
References: Bhidayasiri R, Phuenpathom W, Tan AH, Leta V, Phumphid S, Chaudhuri KR and Pal PK (2022) Management of dysphagia and gastroparesis in Parkinson’s disease in real-world clinical practice – Balancing pharmacological and non-pharmacological approaches.
Front. Aging Neurosci. 14:979826. doi: 10.3389/fnagi.2022.979826
Soliman,H.;Coffin,B.; Gourcerol, G. Gastroparesis in Parkinson Disease: Pathophysiology, and Clinical Management. Brain Sci. 2021,11,831. https://doi.org/ 10.3390/brainsci11070831Öthman,M.;Widman,E.; Nygren, I.; Nyholm, D. Initial Experience of the Levodopa–Entacapone–Carbidopa Intestinal Gel in Clinical Practice. J. Pers.Med.2021,11,254. https:// doi.org/10.3390/jpm11040254
To cite this abstract in AMA style:
G. Tabar Comellas, MI. Morales Casado, JC. Segundo-Rodríguez, N. Lopez Ariztegui. Clinical Improvement and drastic reduction of Equivalent Dose of Levodopa (LEDD) in an Advanced Parkinson’s Disease Patient after Levodopa/Entacapone/Carbidopa Intestinal Gel (LECIG) Treatment [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-improvement-and-drastic-reduction-of-equivalent-dose-of-levodopa-ledd-in-an-advanced-parkinsons-disease-patient-after-levodopa-entacapone-carbidopa-intestinal-gel-lecig-treatment/. Accessed December 15, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-improvement-and-drastic-reduction-of-equivalent-dose-of-levodopa-ledd-in-an-advanced-parkinsons-disease-patient-after-levodopa-entacapone-carbidopa-intestinal-gel-lecig-treatment/