Category: Neuroimaging (Non-PD)
Objective: To describe the clinical features and the metabolic patterns assessed by the brain [18F] FDG-PET in a cohort of PSP patients with or without ventricular dilatation.
Background: Brain ventricular enlargement is a frequent finding in neurodegenerative diseases such as PSP. This seems to be related to an underlying neurodegenerative process and can precede the typical manifestations of the disease. Brain MRI abnormalities in PSP patients are different in the distinct subtypes, but the correlation of ventriculomegaly with clinical manifestations has not been described.
Method: This retrospective study analyzed 36 adults (mean age 70.4 ± 12.1 years) with probable PSP at Clínica Universidad de Navarra from January 2020 to January 2024. Patients met MDS-PSP criteria, supported by FDG-PET brain scans. All underwent brain MRI and FDG-PET scans. The brain 18F-FDG-PET patterns underwent visual analysis by a nuclear medicine specialist, who scrutinized regions of interest (ROI). Ventriculomegaly was defined by Evans Index >0.3 and Callosal Angle <100º, categorizing patients into two groups of 18 based on ventricular enlargement presence.
Results: Among 36 patients analyzed, freezing of gait (83%) was the most common clinical feature in PSP patients with ventriculomegaly, followed by falls. Notably, the PSP-pure akinesia with gait freezing (PAGF) was the predominant variant of these cases. Conversely, in the PSP group without ventriculomegaly, postural instability (39%) and falls (33%) were the primary symptoms, with the PSP-Richardson syndrome prevailing in most cases.
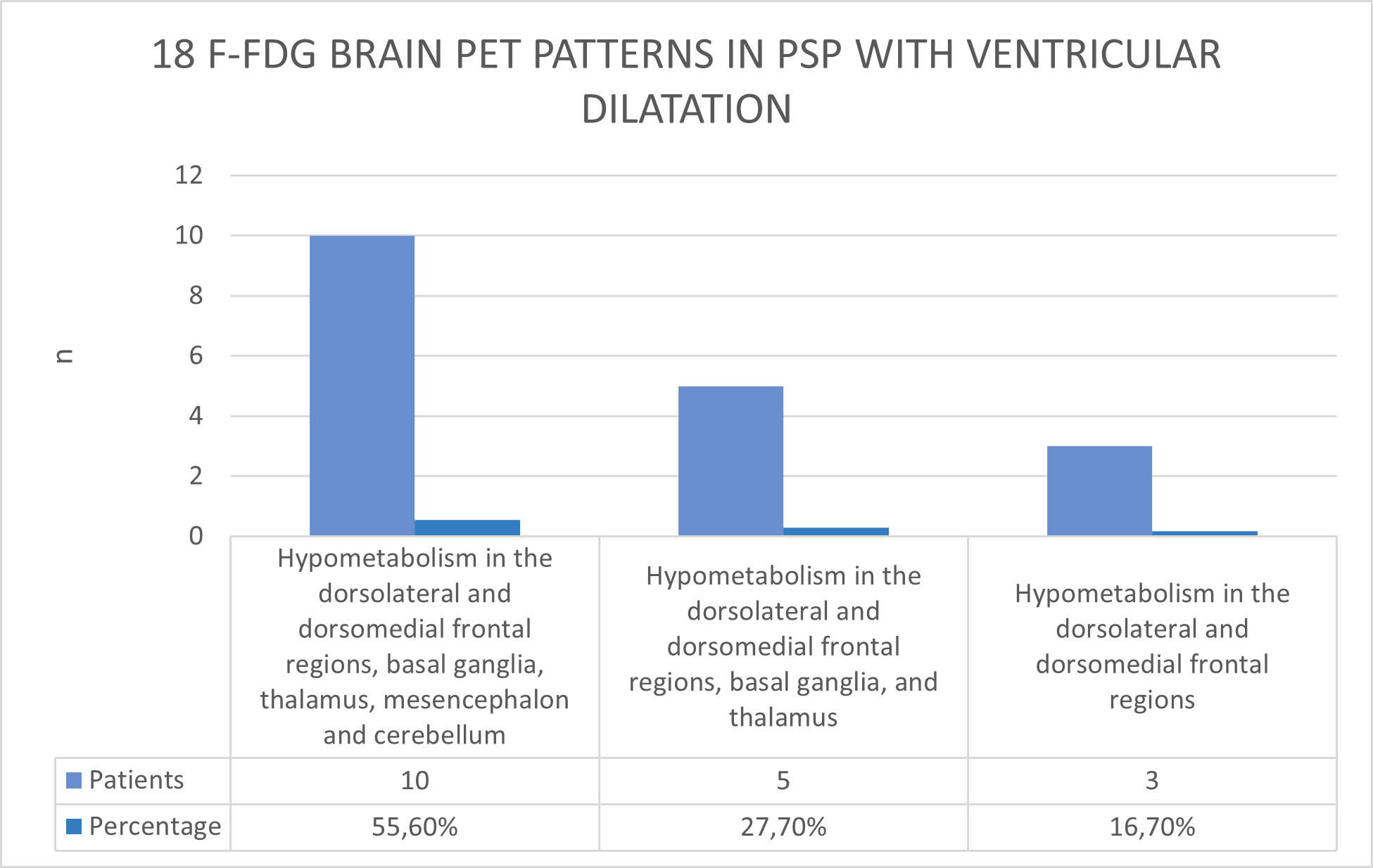
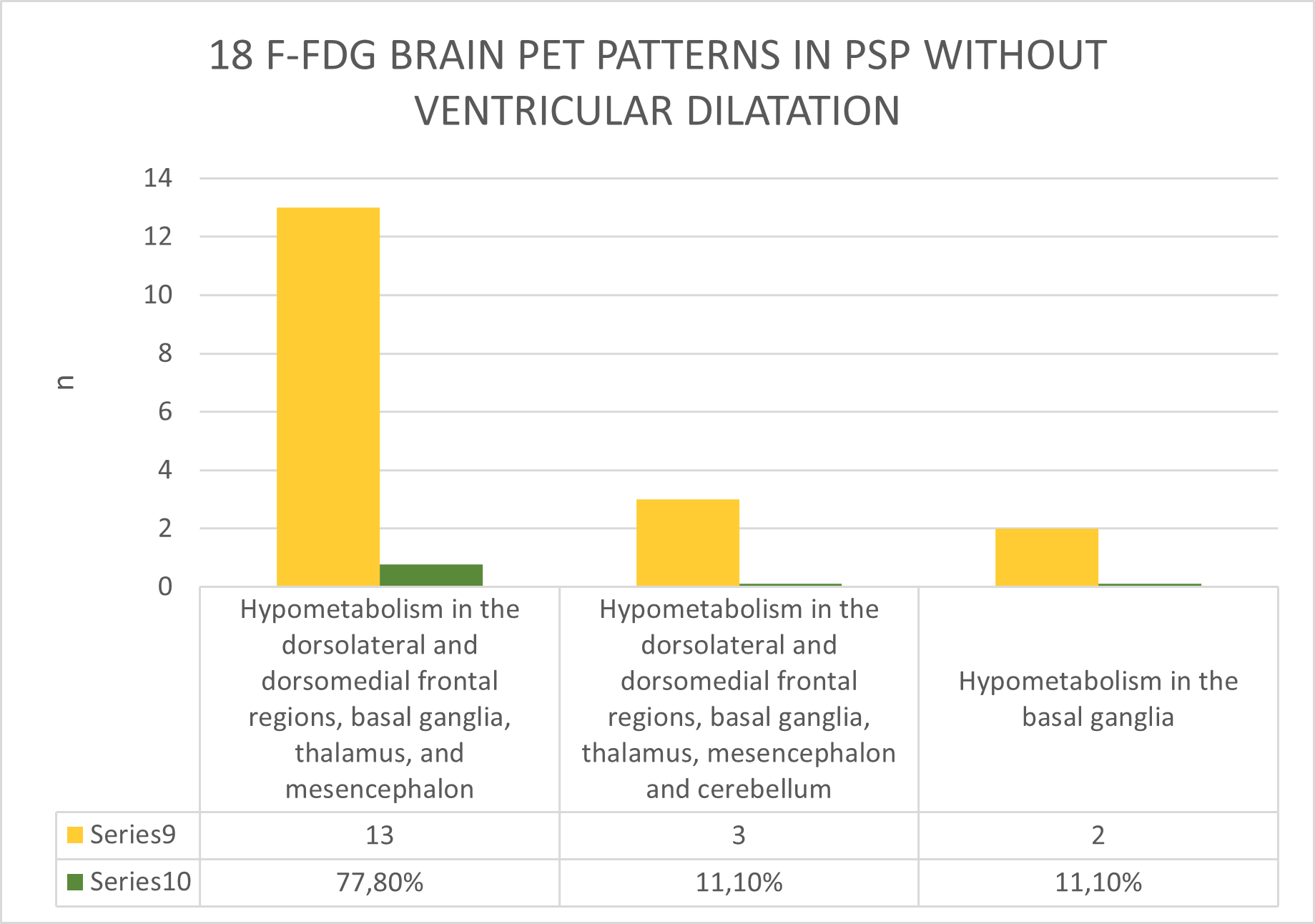
Brain metabolic patterns differed between the two groups. Dorsolateral and dorsomedial frontal cortex, with basal ganglia, thalamus, mesencephalon, and cerebellum hypometabolism was observed in 55.60% of PSP patients with ventriculomegaly, while dorsolateral and dorsomedial frontal cortex, basal ganglia, thalamus, and mesencephalon hypometabolism was predominant in 77.80% of PSP patients without ventriculomegaly. The remaining patterns in both groups are described in Figures 1 and 2.
Conclusion: Our findings indicate that ventriculomegaly in PSP patients is associated with a different phenotype and metabolic patterns and might indicate a distinct underlying neurodegenerative process.
Figure 1
Figure 2
References: 1. Fu MH, Huang CC, Wu KLH, Chen YF, Kung YC, Lee CC, Liu JS, Lan MY, Chang YY. Higher prevalence of idiopathic normal pressure hydrocephalus-like MRI features in progressive supranuclear palsy: An imaging reminder of atypical parkinsonism. Brain Behav. 2023 Feb;13(2):e2884. doi: 10.1002/brb3.2884. Epub 2023 Jan 12. PMID: 36635882; PMCID: PMC9927835.
2. Ohara M, Hattori T, Yokota T. Progressive supranuclear palsy often develops idiopathic normal pressure hydrocephalus-like magnetic resonance imaging features. Eur J Neurol. 2020 Oct;27(10):1930-1936. doi: 10.1111/ene.14322. Epub 2020 Jun 29. PMID: 32416639.
To cite this abstract in AMA style:
C. Espinoza-Vinces, I. Avilés-Olmos, G. Martí-Andrés, R. Villino-Rodríguez, C. Pérez-Prol, M. Gimeno-Rodríguez, J. Arbizu, MR. Luquin. Clinical features and brain [18F] FDG PET patterns in patients with progressive supranuclear palsy with and without ventricular dilatation [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-features-and-brain-18f-fdg-pet-patterns-in-patients-with-progressive-supranuclear-palsy-with-and-without-ventricular-dilatation/. Accessed January 19, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-features-and-brain-18f-fdg-pet-patterns-in-patients-with-progressive-supranuclear-palsy-with-and-without-ventricular-dilatation/