Session Information
Date: Monday, June 5, 2017
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: To compare patients with mild and severe daytime somnolence using cut-off values from item 15 of the Parkinson’s disease (PD) sleep scale (PDSS).
Background: Although risk factors for sudden onset of sleep (SoS) and somnolence in PD have been studied, large scale data is missing.
Methods: We classified 658 patients with PD into 3 subgroups based on PDSS item15 scores, mild (>7) moderate (5-7) and severe (<5).
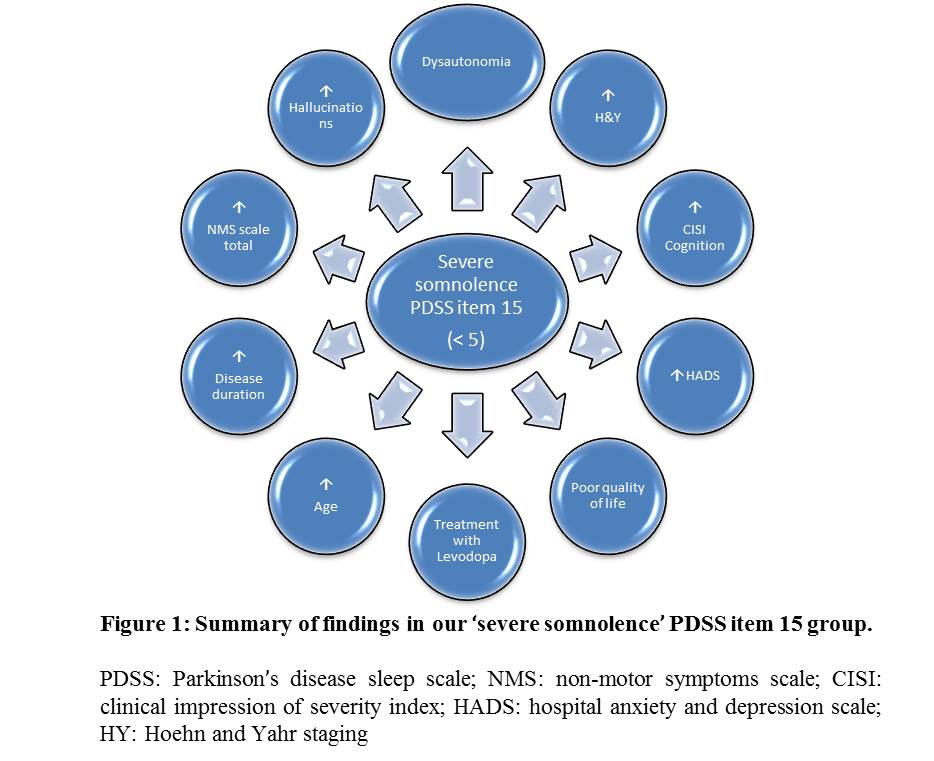
Results: Severe sleepiness was present in 38.8% (N=255). Compared to patients with mild sleepiness (N=360), those patients were of older age (mean in years 68.5±10.15 versus 64.8±11.4), had a longer disease duration (mean in years 5.8±5.1 versus 4.9±5), higher Hoehn and Yahr state (median 3 (1-5) versus 2 (0-5)), higher non motor symptoms (NMS) scale total score (63±41.6 versus 39.1±31.3), higher rate of hallucinations on NMS scale (0.8±1.8 versus 0.2±0.9), more autonomic dysfunction on NMS scale (16.8±12.7 versus 10.8±9.9), higher clinical impression of severity index cognition (1±1.1 versus 0.4±0.7), higher Hospital anxiety and depression scale (13.4 ±8 versus 9.8±6.3) and poorer quality of life (mean PDQ-8 total score 10.25±6.5 versus 6.6±5.5). 75.7% of patients with severe sleepiness were treated with Levodopa compared to 58.6 % with mild sleepiness (figure 1). Several patients had sudden onset of sleep.
Conclusions: Severe somnolence likely reflects a specific subtype (Park sleep) of PD (1). There is sensitivity to dopaminergic drugs and a higher NMS burden. These observations have clinical implications regarding personalised medication strategies in this subgroup.
References: (1) Sauerbier A, Jenner P, Todorova A, Chaudhuri KR. Non motor subtypes and Parkinson’s disease. Parkinsonism Relat Disord. 2016 Jan;22 Suppl 1:S41-6. doi: 10.1016/j.parkreldis.2015.09.027. Epub 2015 Sep 11.
Acknowledgements: We are sincerely grateful to the UK NILS collaborators and the MDS NM PD Study Group
To cite this abstract in AMA style:
R. Taddei, A. Sauerbier, M. Qamar, K. Ray Chaudhuri. Clinical correlates of severe somnolence in Parkinson’s disease: results from an international naturalistic non-motor symptoms cohort [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/clinical-correlates-of-severe-somnolence-in-parkinsons-disease-results-from-an-international-naturalistic-non-motor-symptoms-cohort/. Accessed December 20, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-correlates-of-severe-somnolence-in-parkinsons-disease-results-from-an-international-naturalistic-non-motor-symptoms-cohort/