Category: Parkinson's Disease: Neuroimaging
Objective: To define and cross-validate the glucose metabolism abnormalities related to Parkinson’s Disease (PD), and to analyze pattern relationship with clinical phenotype
Background: In PD, spatial covariance analysis of FDG-PET data has consistently defined a distinctive PD-related metabolic pattern (PDRP). However, the clinical correlates of the metabolic network are still limited, at least partly, by small sample-size studies [1-4]
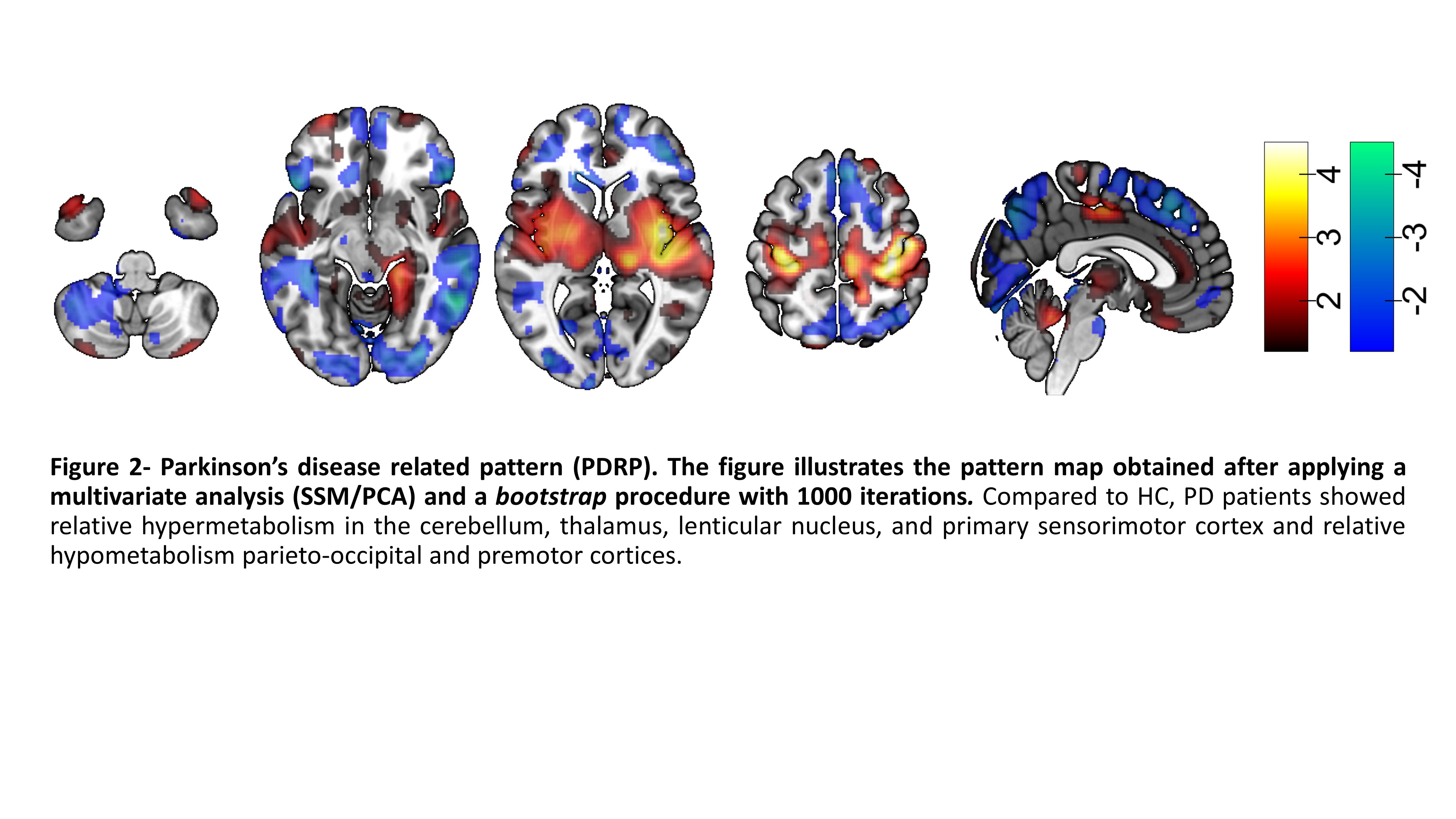
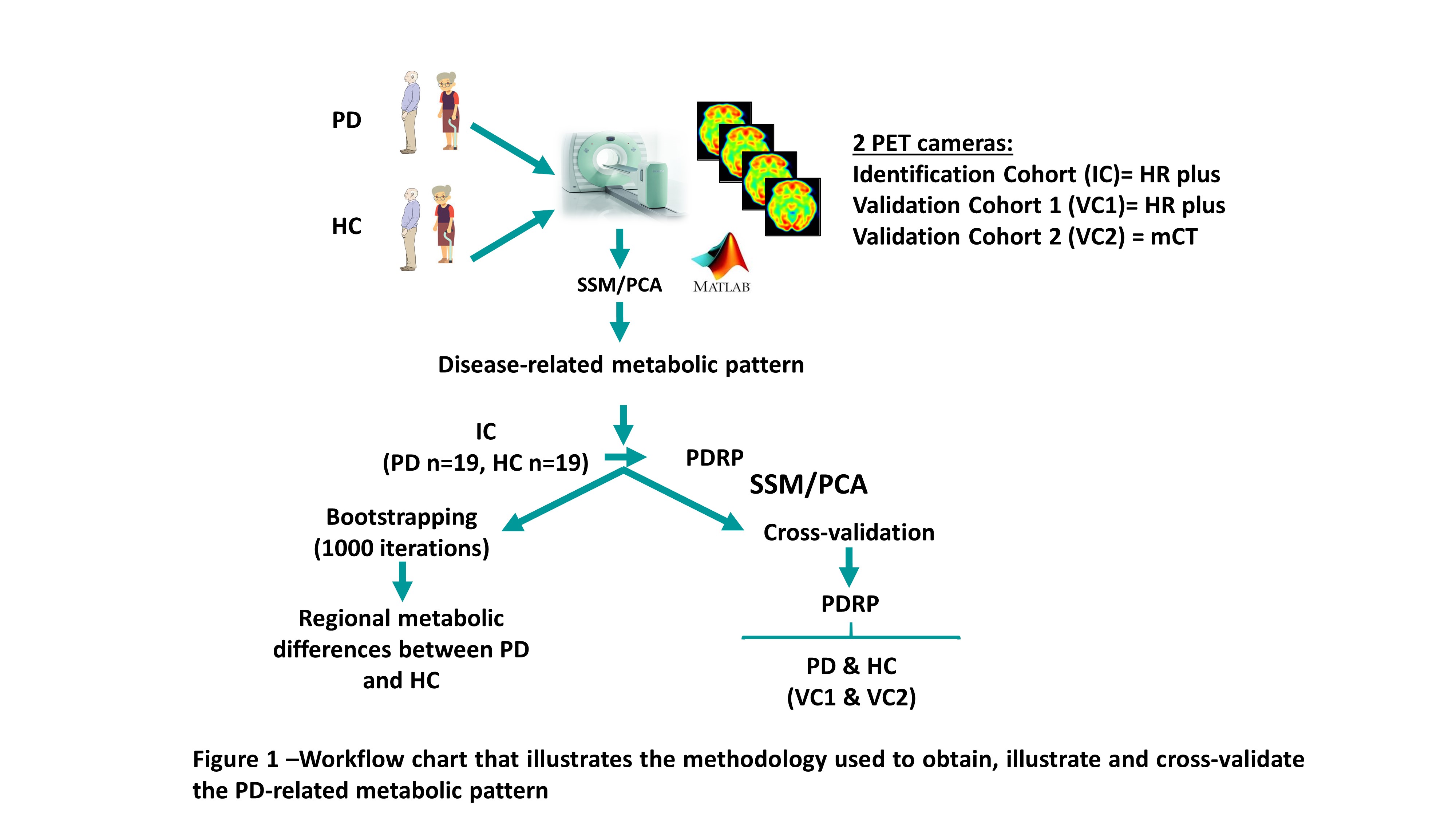
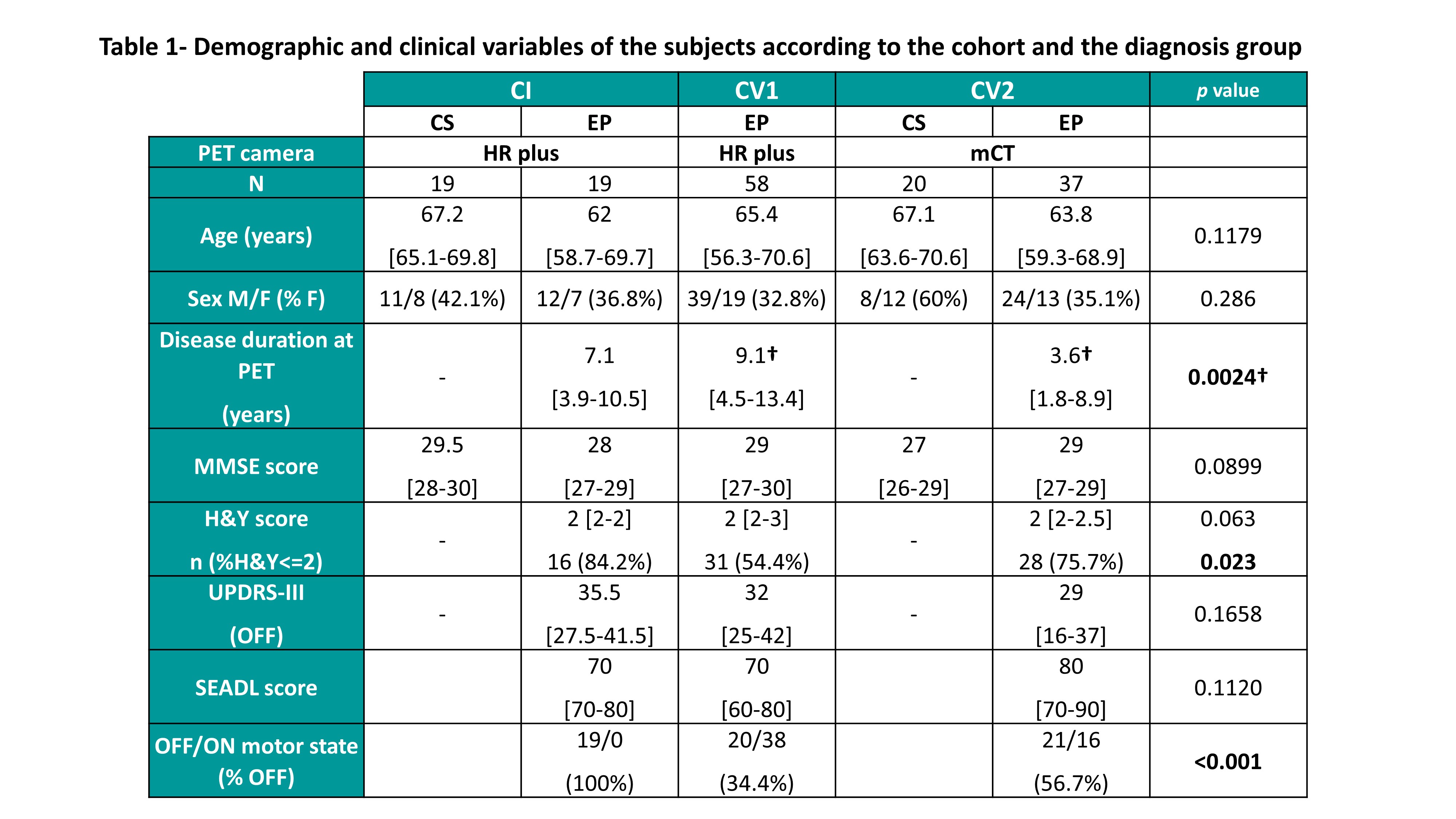
Method: We performed a retrospective, cohort study on 114 PD patients who were referred for an FDG-PET scan. We also included 39 healthy controls (HC). We defined one identification cohort (IC)(PD n=19, HC n=19) and two validation cohorts (VC) based on the PET-camera and motor state (VC1: PD n=58; VC2: PD n=37, HC n=20). We analyzed the regional differences in metabolism between the groups using the Scaled Subprofile Model/Principal Component Analysis (SSM/PCA) and obtained a PDRP. Then, we cross-validated the PDRP in independent populations at the individual level (Figure 1). Moreover, we analyzed the relationship between individual PDRP expression and clinical variables.
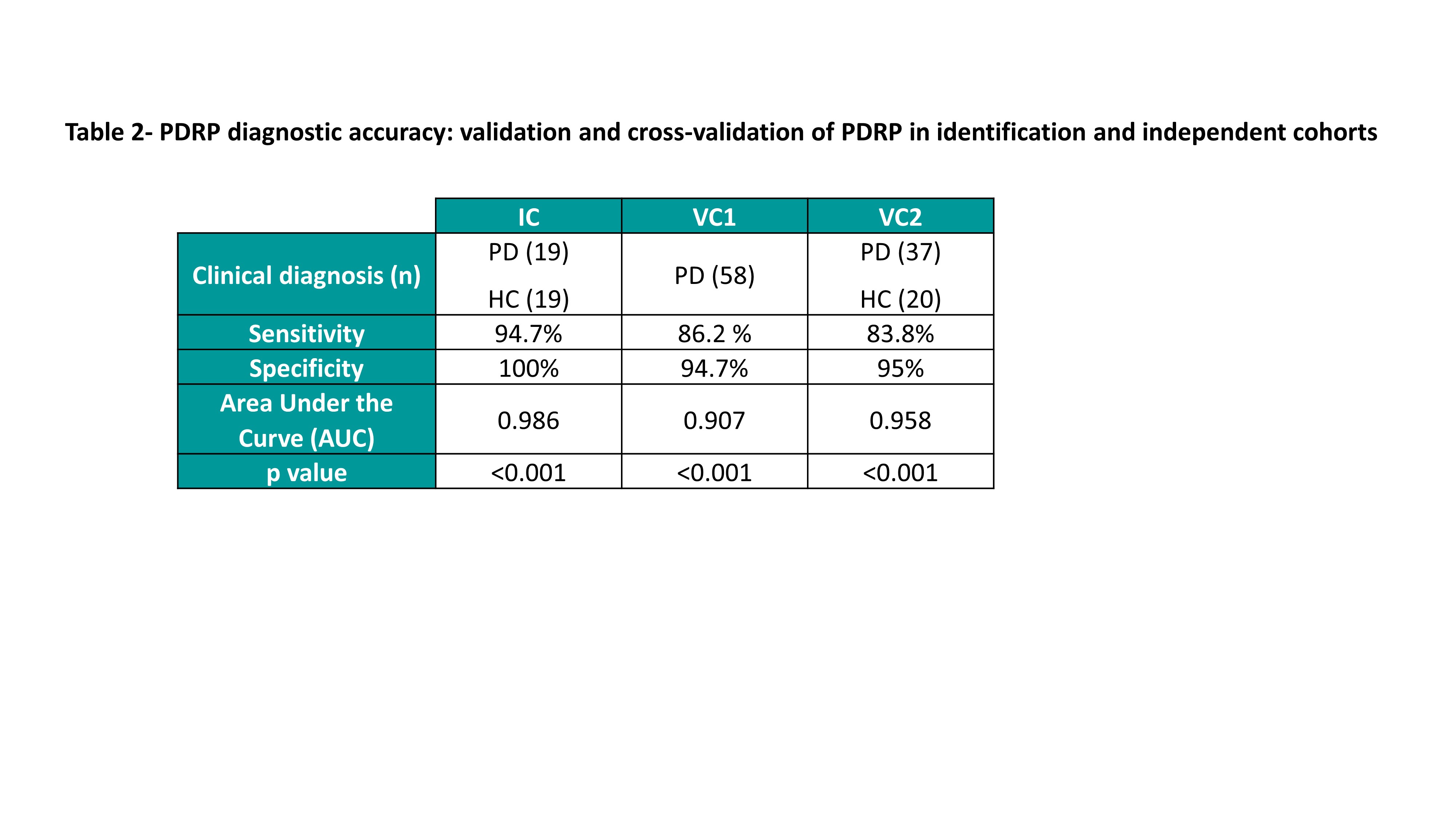
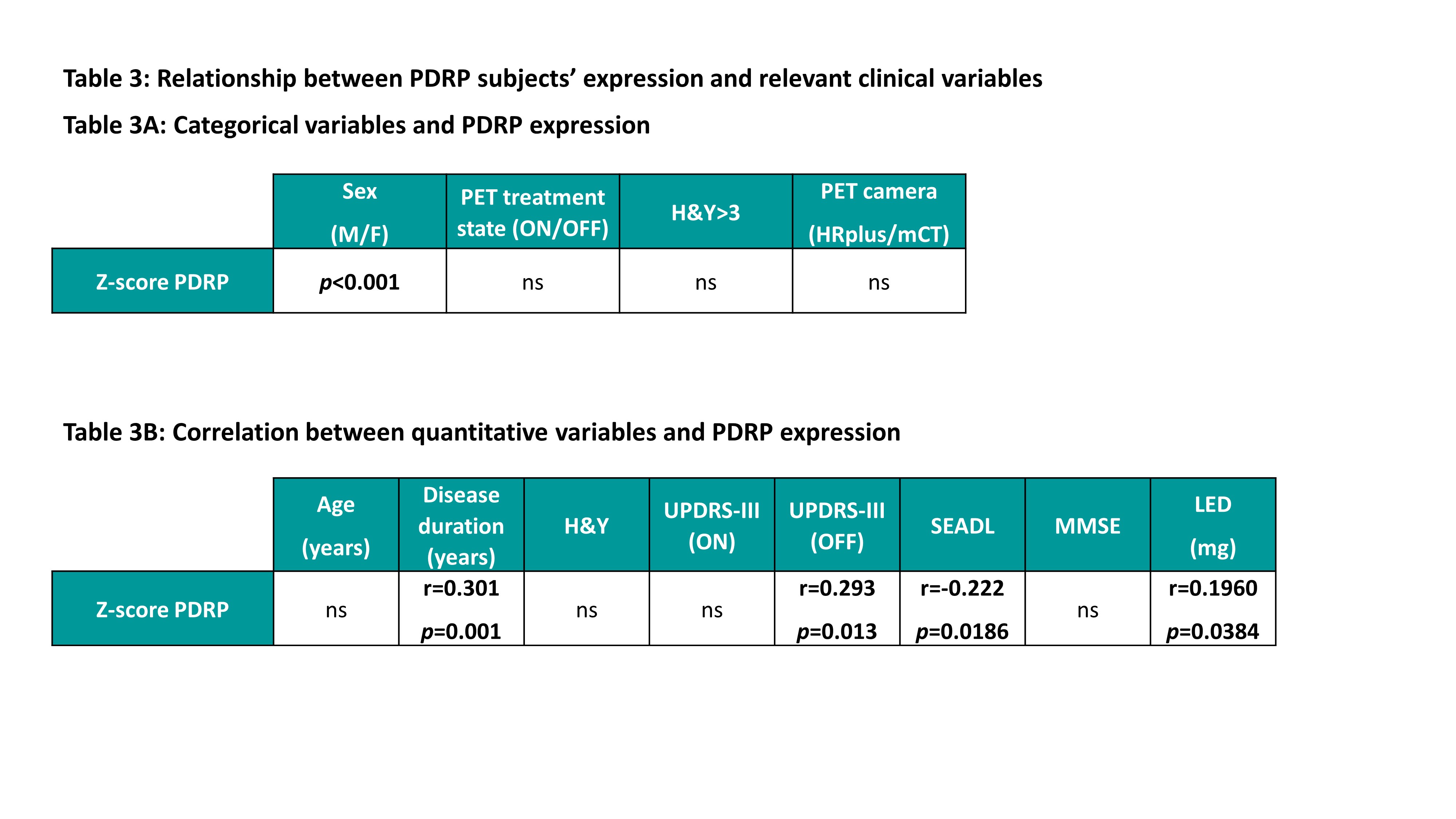
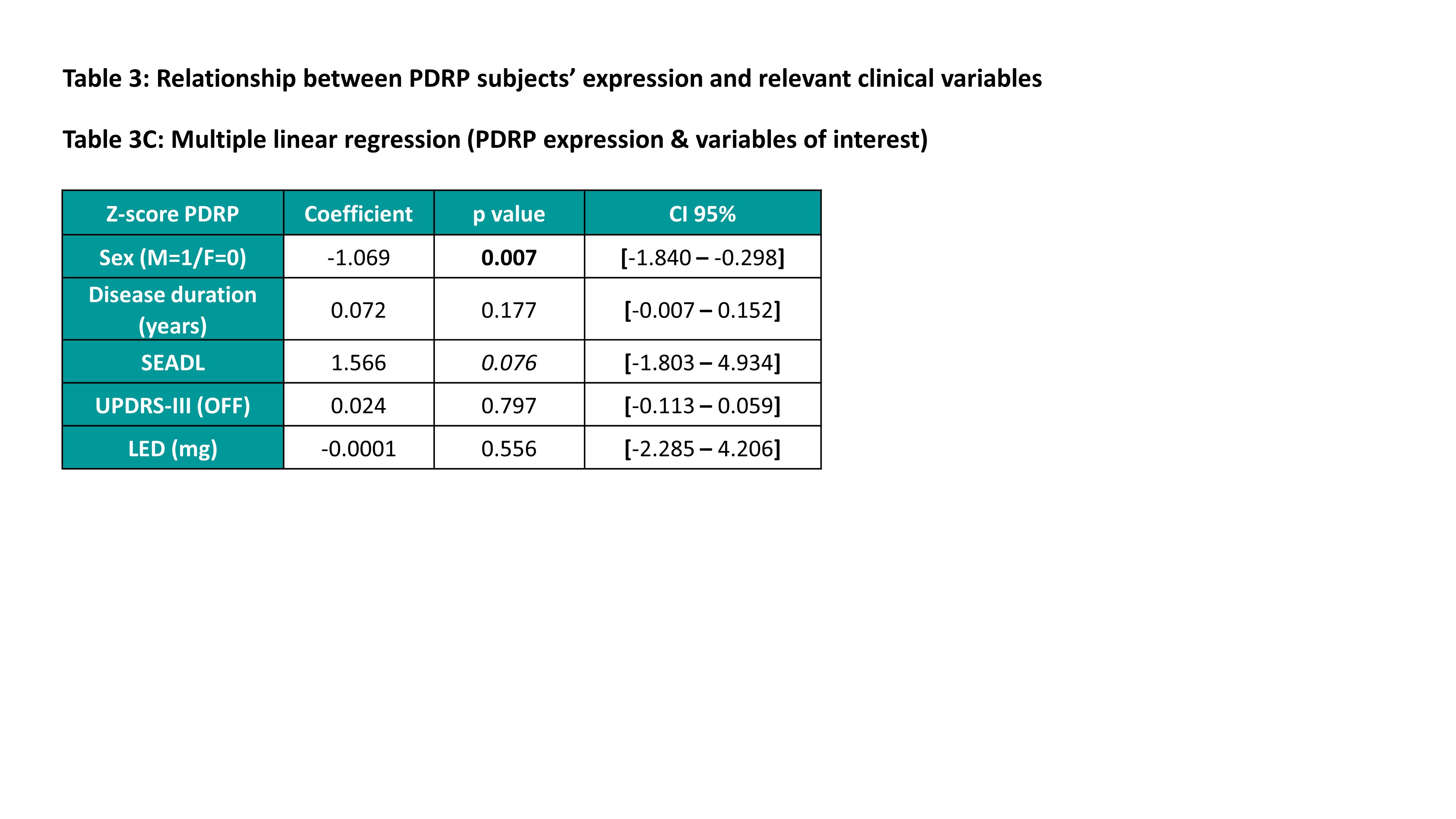
Results: There were no significant differences in age, sex, or cognitive, functional, and motor scores among the cohorts (Table 1). Figure 2 illustrates the PDRP pattern map obtained. Moreover, the pattern showed an optimal diagnostic accuracy to distinguish between PD and HC subjects in both IC and VC (Table 2). Furthermore, we observed a higher pattern expression in males than females. There were also positive correlations between the PDRP expression and duration of disease, UPDRS-III (OFF state) and LED, and a negative correlation with the functional state. However, after multiple linear regression, only the sex showed an independent and significant relationship with the PDRP expression (Table 3A-C).
Conclusion: The glucose metabolism assessed by FDG-PET is a useful and reproducible supportive diagnostic tool for PD patients. Moreover, the PDRP expression shows a correlation with variables related to disease severity. Remarkably, gender shows an independent impact on pattern expression, which may be due to gender-related differences in disease pathophysiology [5] and may explain why males tend to have more severe symptoms and greater speed of progression.
References: [1] K.A. Schindlbeck, D. Eidelberg, Network imaging biomarkers: insights and clinical applications in Parkinson’s disease, Lancet Neurol. 17 (2018) 629–640. doi:10.1016/S1474-4422(18)30169-8. [2] S.K. Meles, R.J. Renken, M. Pagani, L.K. Teune, D. Arnaldi, S. Morbelli, F. Nobili, T. van Laar, J.A. Obeso, M.C. Rodríguez-Oroz, K.L. Leenders, Abnormal pattern of brain glucose metabolism in Parkinson’s disease: replication in three European cohorts, Eur. J. Nucl. Med. Mol. Imaging. 47 (2020) 437–450. doi:10.1007/s00259-019-04570-7. [3] K. Asanuma, C. Tang, Y. Ma, V. Dhawan, P. Mattis, C. Edwards, M.G. Kaplitt, A. Feigin, D. Eidelberg, Network modulation in the treatment of Parkinson ’ s disease, (2006) 2667–2678. doi:10.1093/brain/awl162. [4] J.H. Ko, A. Katako, M. Aljuaid, A.L. Goertzen, A. Borys, D.E. Hobson, S.M. Kim, C.S. Lee, Distinct brain metabolic patterns separately associated with cognition, motor function, and aging in Parkinson’s disease dementia, Neurobiol. Aging. 60 (2017) 81–91. doi:10.1016/j.neurobiolaging.2017.08.020. [5] C. Tremblay, N. Abbasi, Y. Zeighami, Y. Yau, M. Dadar, S. Rahayel, A. Dagher, Sex effects on brain structure in de novo Parkinson’s disease: a multimodal neuroimaging study, Brain. (2020). doi:10.1093/brain/awaa234.
To cite this abstract in AMA style:
G. Martí-Andrés, R. Valentí, E. Prieto, M. Riverol, MR. Luquin, J. Arbizu. Clinical correlates of Parkinson’s disease metabolic pattern: not only a diagnostic tool [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-correlates-of-parkinsons-disease-metabolic-pattern-not-only-a-diagnostic-tool/. Accessed December 26, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-correlates-of-parkinsons-disease-metabolic-pattern-not-only-a-diagnostic-tool/