Category: Huntington's Disease
Objective: To assess olfactory dysfunction in patients with HD and correlate the degree of olfactory dysfunction with symptomatic domains of HD.
Background: Olfactory dysfunction is involved in many neurodegenerative diseases, including PD and AD. HD patients have deficits in detecting, recognizing, and recalling odors [1], even before cognitive and motor abnormalities [2]. Screening for olfactory problems in HD is not necessary for diagnosis, given the wide availability and convention of genetic testing, yet, this approach could help determine disease progression and treatment response. Indeed, a significant annualized rate of olfactory decline has been described in patients with HD. However, no additional correlations were measured between olfaction and other motor or cognitive domains [3]. Despite significant evidence indicating olfactory dysfunction in HD, the studies have been heterogenous and used screening tests unsuitable for testing patients of varying cultures. Therefore, we proposed the current research to obtain better information regarding olfactory dysfunction in HD and its association with motor, cognitive, and behavioral symptoms.
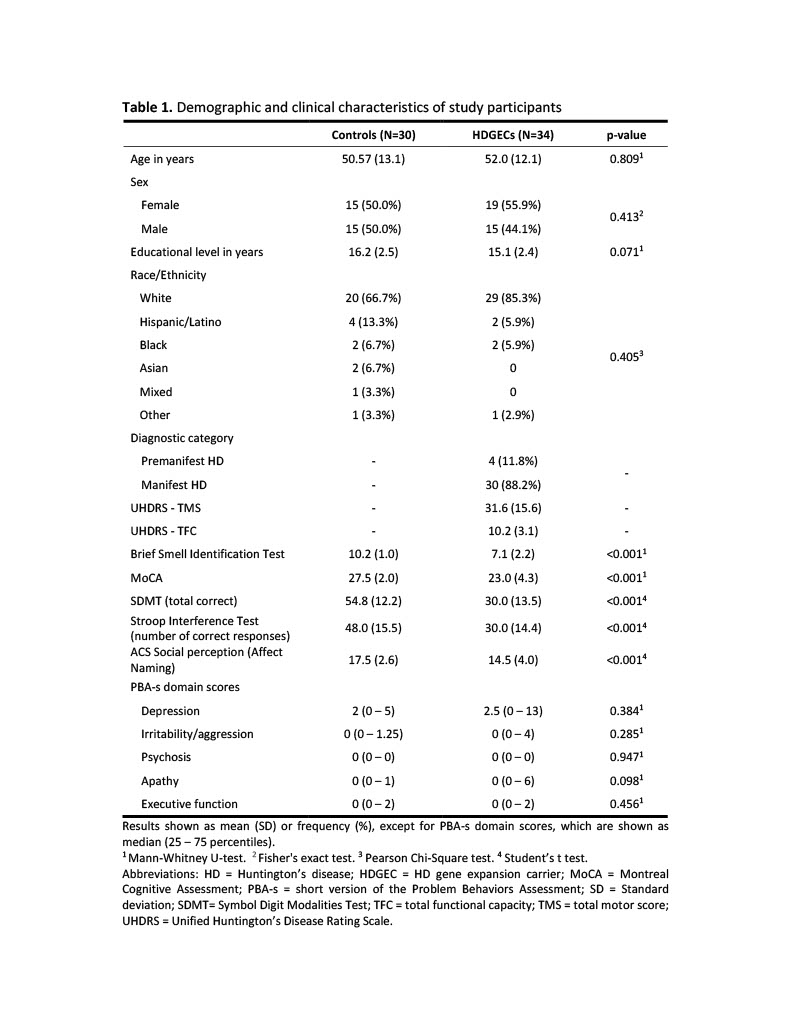
Method: Cross-sectional study of HD gene expansion carriers (HDGECs) who attend the UTHealth Huntington’s Disease Society of America Center of Excellence and a group of controls. Participants underwent the 12-item Brief Smell Identification Test (BSIT), which takes into account cultural differences in odor identification, and a comprehensive clinical assessment that included motor (UHDRS), cognitive [MoCA, SDMT, Stroop test, and Advanced Clinical Solutions (ACS) Social Perception – Affect Naming], and behavioral (Problem Behaviors Assessment) symptoms.
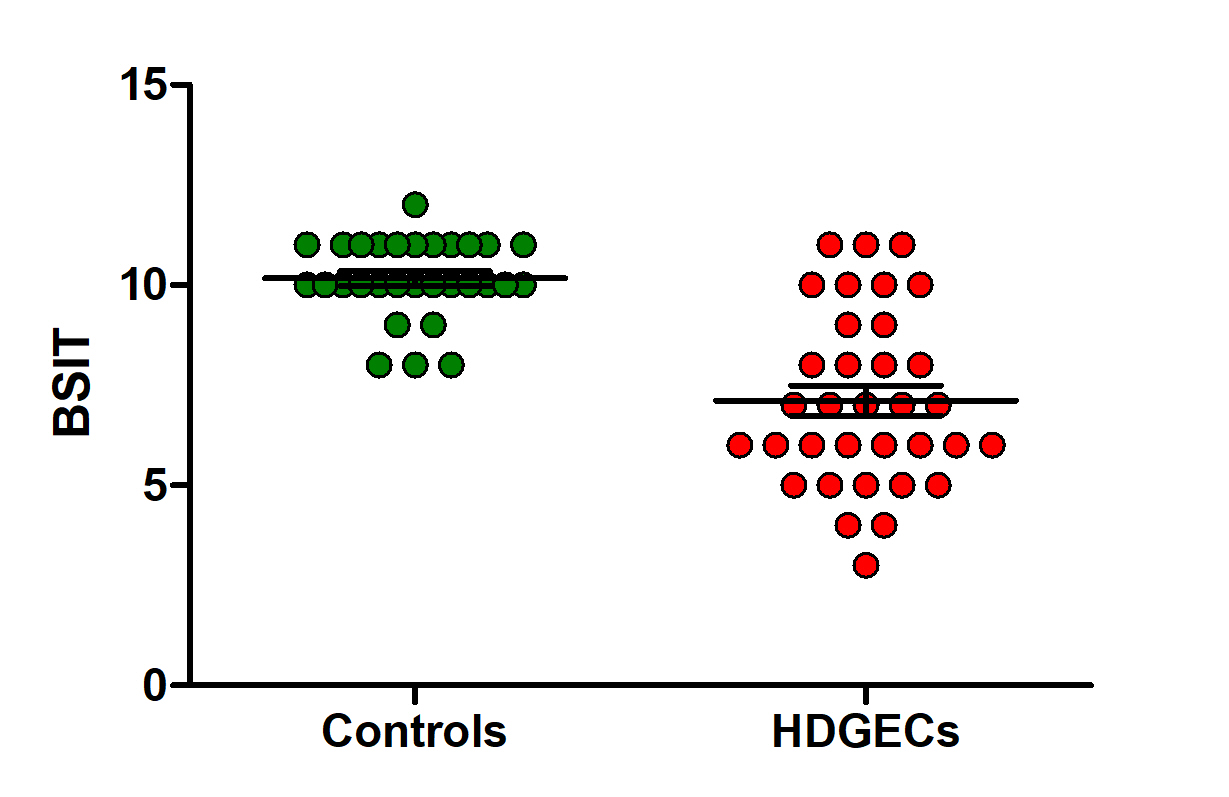
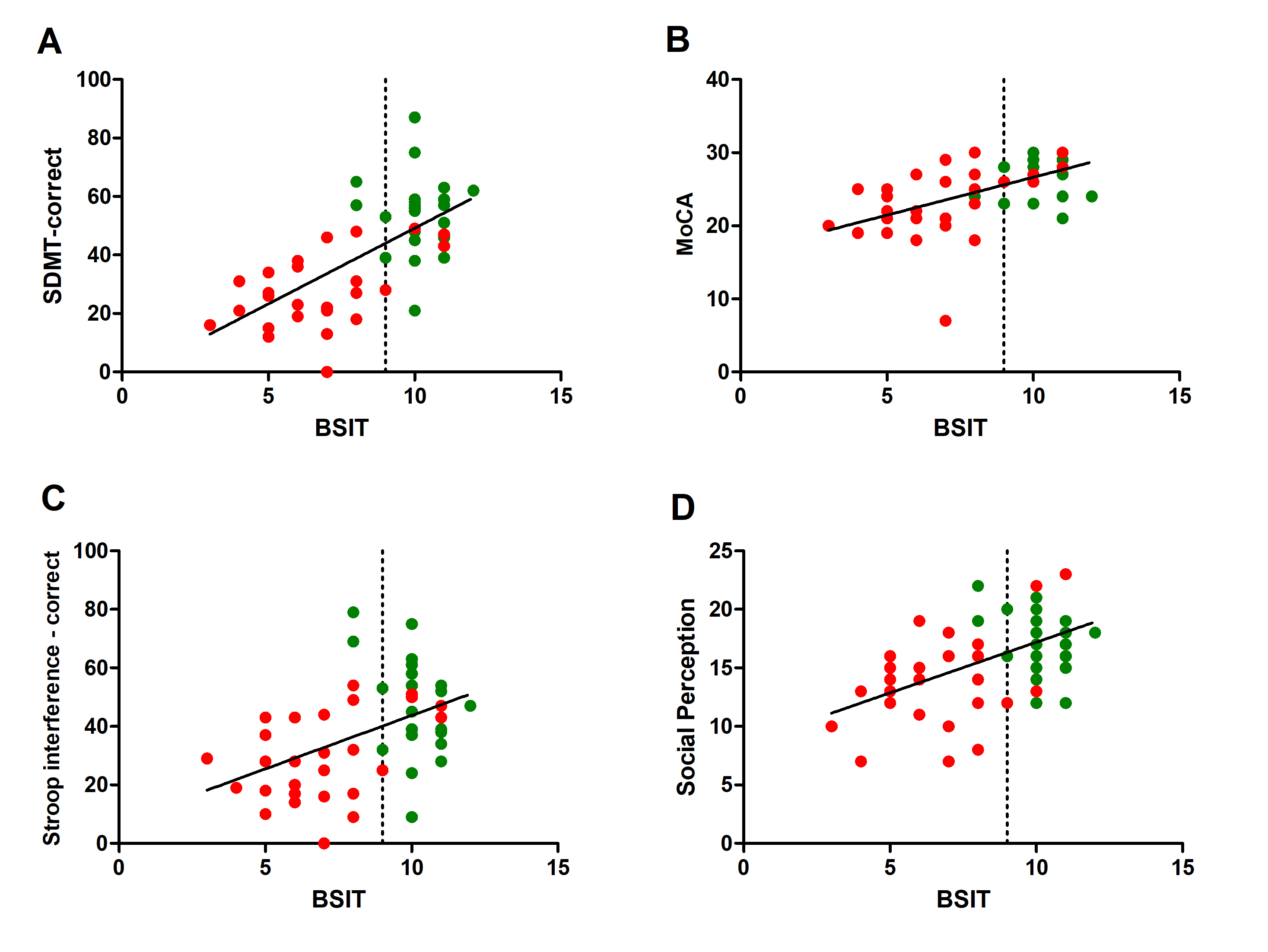
Results: 34 HDGECs and 30 controls completed the study procedures. A general description of the study population is provided in Table 1 [table1]. HDGECs present a significant impairment in odor detection, as demonstrated by lower scores in the BSIT compared to controls (Fig. 1) [figure1]. In addition, we found significant correlations between BSIT and the scores in all cognitive tests (Fig. 2) [figure2]. When the groups were stratified, these correlations remained significant among HDGECs, but not among controls.
Conclusion: DGECs present olfactory impairment that is strongly associated with cognitive performance. Olfactory dysfunction may be a good predictor of HD progression. Longitudinal studies are needed to confirm our findings.
References: [1] Bacon Moore, A. S., Paulsen, J. S., & Murphy, C. (1999). A test of odor fluency in patients with Alzheimer’s and Huntington’s disease. Journal of clinical and experimental neuropsychology, 21(3), 341–351.
[2] Dayalu, P., & Albin, R. L. (2015). Huntington disease: pathogenesis and treatment. Neurologic clinics, 33(1), 101–114.
[3] Tabrizi, S. J., Scahill, R. I., Durr, A., Roos, R. A. C., Leavitt, B. R., Jones, R., et al. (2011). Biological and clinical changes in premanifest and early stage Huntington’s disease in the TRACK-HD study: The 12-month longitudinal analysis. The Lancet Neurology, 10(1), 31–42.
To cite this abstract in AMA style:
N. Rocha, J. Patino, S. Abdollah Zadegan, H. Coco, A. Liang, F. Ramirez, E. Furr Stimming. Clinical correlates of olfactory dysfunction in Huntington’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-correlates-of-olfactory-dysfunction-in-huntingtons-disease/. Accessed January 4, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-correlates-of-olfactory-dysfunction-in-huntingtons-disease/