Category: Parkinson's Disease: Neuroimaging
Objective: To assess clinical and radiological risk factors of mortality in a cohort of patients with a clinical diagnosis of Parkinson’s disease (PD) according to the MDS-PD criteria.
Background: Many studies have revealed clinical factors associated with higher risk of mortality in PD patients [1-3]. Less is known about the impact of FDG-PET findings on survival.
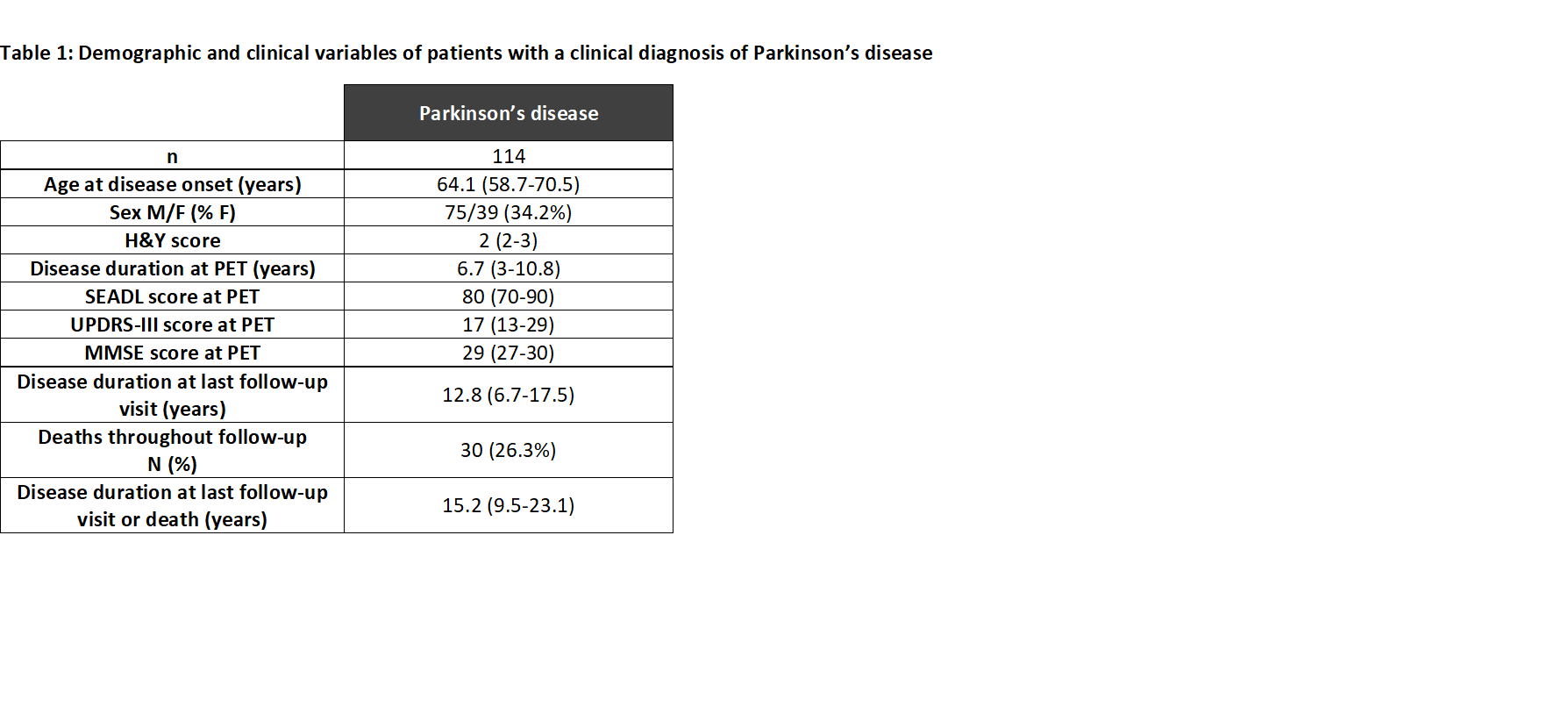
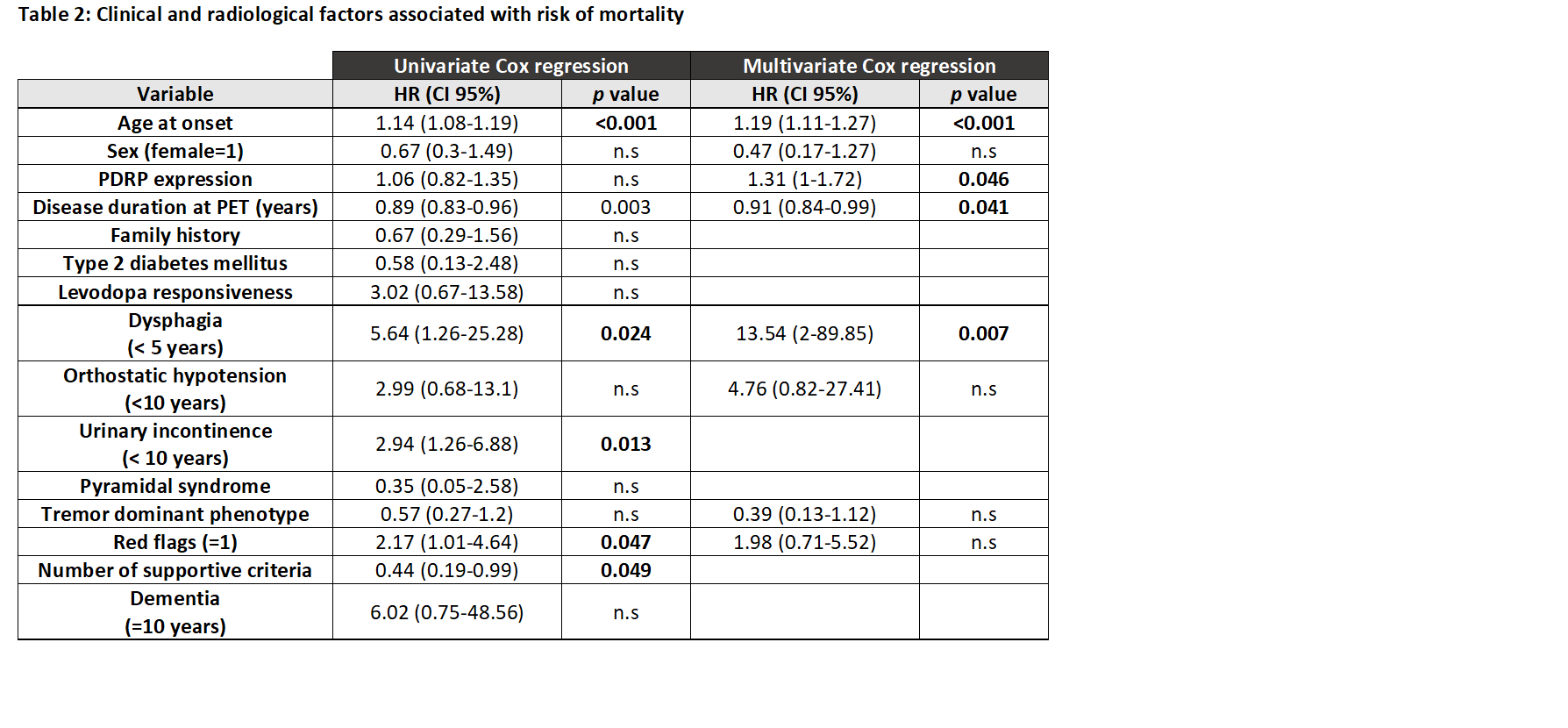
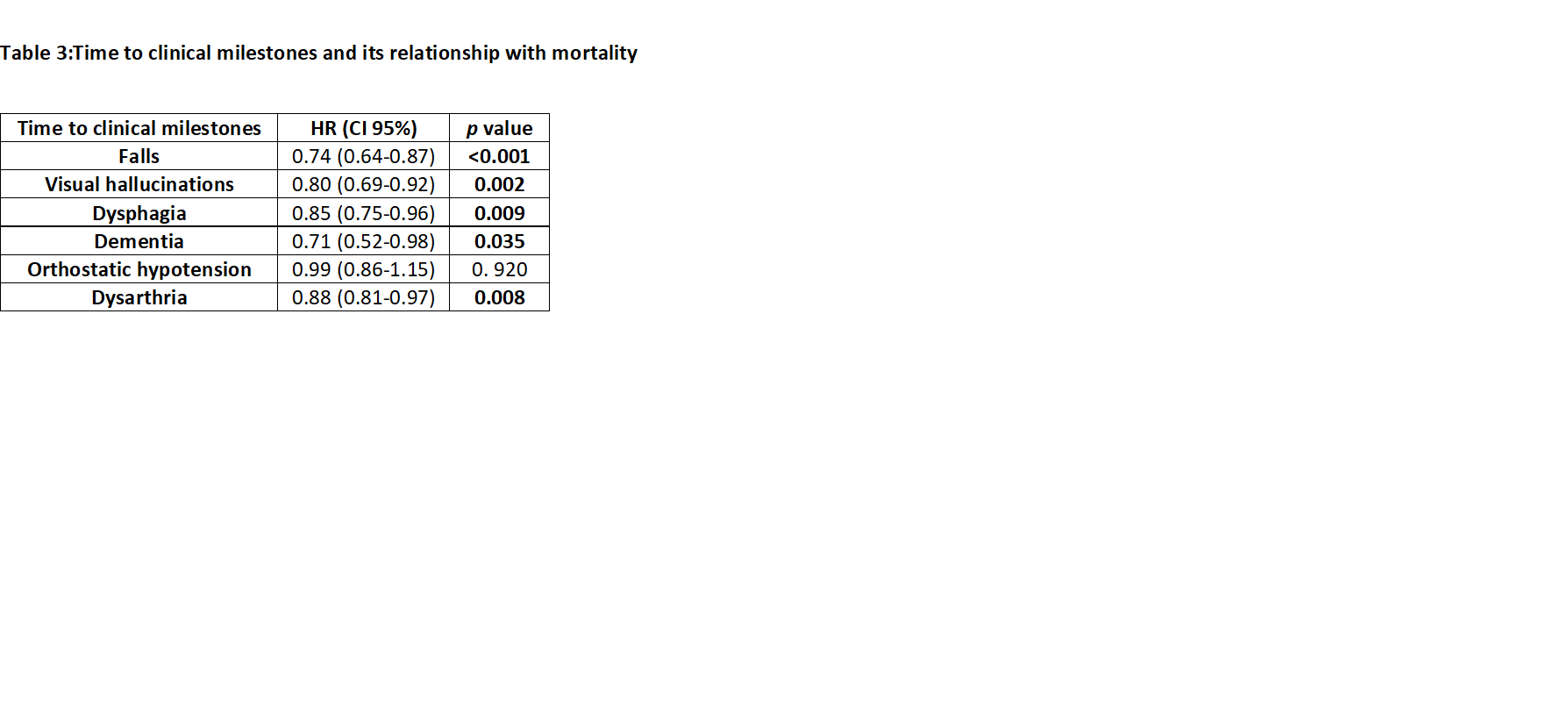
Method: We performed a retrospective cohort study and included a total of 114 PD patients who had been referred for an FDG-PET scan throughout the disease course. We performed a systematic review of medical charts and obtained clinical and radiological variables, including the date of death or last follow-up visit date in subjects who were alive in December 2022. We included the individual expression of a predefined PD-related pattern (PDRP)[x] obtained using a multivariate Scaled Subprofile Model/Principal Component Analysis (SSM/PCA) into FDG-PET scans. A Kaplan-Meier test was performed to calculate the median of survival. The risk of death in PD patients was calculated using a Cox proportional hazard model in univariate analysis. We selected variables that had previously been determined as predictors of survival. Those variables associated with a change in the risk of death and those previously described as clinically relevant were entered into the multivariate Cox regression model. Moreover, we analyzed the impact on the risk of death at the time of onset of preselected clinical milestones.
Results: Clinical variables are described in [Table1]. PD patients were followed up for a median of 13 years when a total of 30 PD patients died. The median survival was 26.9 years. Increased age at disease onset, presence of dysphagia in the first 5 years, lower disease duration at PET, and higher expression of PDRP in FDG-PET imaging were independent risk factors of mortality [Table 2]. Moreover, lower time to develop falls, visual hallucinations, dysphagia, dementia, or dysarthria were associated with an increased risk of mortality [Table 3].
Conclusion: Older age at onset, early appearance of dysphagia, and higher expression of PDRP in FDG-PET imaging have a negative impact on survival. Moreover, the earlier patient develops symptoms of advanced PD the higher the risk of mortality will be.
References: [1] Macleod AD, Taylor KSM, Counsell CE. Mortality in Parkinson’s disease: A systematic review and meta‐analysis. Mov Disord [Internet]. 2014 Nov 13;29(13):1615–22. Available from: https://onlinelibrary.wiley.com/doi/10.1002/mds.25898
[2] van Rumund A, Esselink RAJ, Berrevoets-Aerts MB, Otto M, Bloem BR, Verbeek MM. Factors associated with mortality in early stages of parkinsonism. npj Park Dis [Internet]. 2022 Jun 2;8(1):67. Available from: https://www.nature.com/articles/s41531-022-00329-4
[3] Gonzalez MC, Dalen I, Maple-Grødem J, Tysnes O-B, Alves G. Parkinson’s disease clinical milestones and mortality. npj Park Dis [Internet]. 2022 May 12;8(1):58. Available from: https://www.nature.com/articles/s41531-022-00320-z
[4] Martí-Andrés, G., et al. Clinical correlates of Parkinson’s disease metabolic pattern: not only a diagnostic tool. 25th international congress of Parkinson ́s disease and movement disorders. MDS virtual congress 2020.
To cite this abstract in AMA style:
G. Martí-Andrés, E. Prieto-Azcárate, CA. Espinoza-Vinces, M. Riverol, J. Arbizu, R. Luquin. Clinical and radiological factors associated with mortality in Parkinson’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-and-radiological-factors-associated-with-mortality-in-parkinsons-disease/. Accessed February 19, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-and-radiological-factors-associated-with-mortality-in-parkinsons-disease/