Category: Other
Objective: The objective of the study was to evaluate the longitudinal changes in the choroid layer of the eye in patients with Parkinson’s disease (PD).
Background: There is definite evidence for the involvement of choroid layer of the eye in Parkinson’s disease (PD). Cross-sectional studies have yielded conflicting results with regard to choroid thickness in PD. [1-4] The only study which longitudinally evaluated the choroid thickness in patients with PD had a very small sample size of seven patients and the choroid thickness at follow-up was not significantly different from that of the baseline. [4]
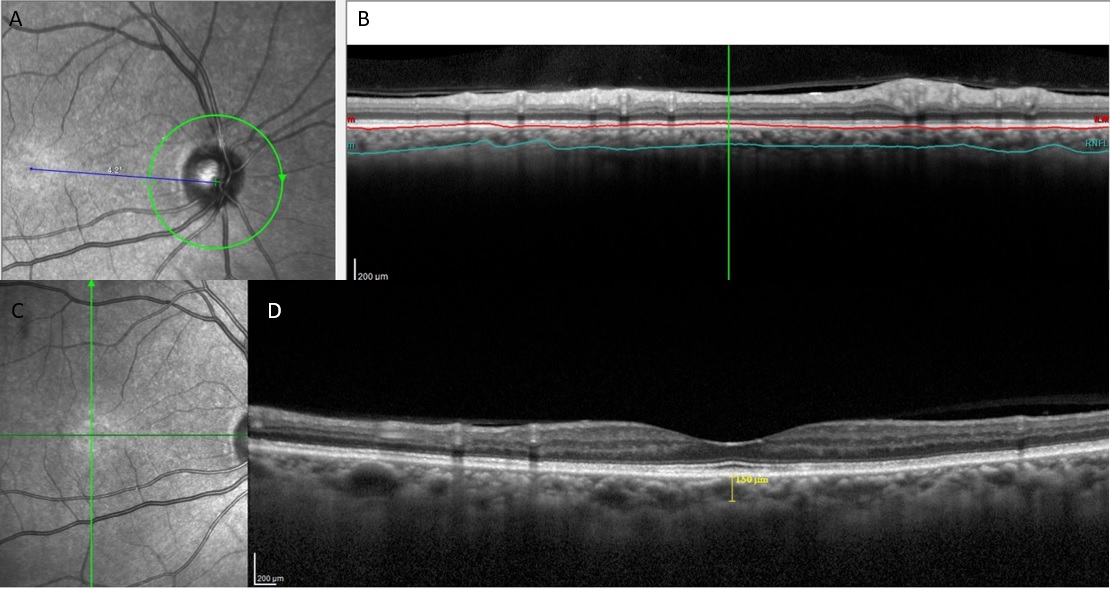
Method: Twelve patients with PD were evaluated at baseline with complete history, clinical examination, Unified Parkinson’s disease Rating Scale (UPDRS) motor part, visual acuity, and subfoveal and peripapillary choroid thickness with spectral domain OCT. [Figure 1: Spectral domain OCT of the Right eye of the patient to show measurement of the Peripapillary choroidal thickness. A, B-. The OCT image depicts the peripapillary choroid thickness (PPCht)-the area between the red line (Brusch membrane) and the green line (lower limit of the choroid). C, D- The OCT image depicting the Subfoveal choroidal thickness] They were evaluated again after a mean duration of 3.7 years. At the time of baseline evaluation, the mean age of the patients was 55.6 ±7.8 years and the mean duration of the disease was 4.5±4.4 years.
Results: The nasal superior, temporal, superotemporal segments of the peripapillary choroid of both the eyes, nasal and nasal inferior segments of the left eye, and the subfoveal choroid thickness of both eyes were found to be significantly thicker during follow-up as compared to baseline. (Table 1) Linear regression analysis revealed that age and UPDRS scores had no impact on the choroidal parameters.
Conclusion: The increase in thickness of the choroid during longitudinal follow-up of patients with Parkinson’s disease is a novel finding. The Choroid, the vascular layer of the eye has autonomic innervation and significant changes in the choroid layer, especially during follow-up could be due to the autonomic dysfunction in Parkinson’s disease (PD). Vascular involvement may also contribute to the pathogenesis of PD.
References: 1. Garcia-Martin E, Jarauta L, Pablo LE, Bambo MP, Ara JR, Martin J, Polo V, Larrosa JM, Vilades E, Ramirez T, Satue M. Changes in peripapillary choroidal thickness in patients with multiple sclerosis. Acta Ophthalmol. 2019 Feb;97(1):e77-e83. doi: 10.1111/aos.13807. Epub 2018 Sep 21. PMID: 30239142.
2. Eraslan M, Cerman E, Yildiz Balci S, Celiker H, Sahin O, Temel A, Suer D, Tuncer Elmaci N. The choroid and lamina cribrosa is affected in patients with Parkinson’s disease: enhanced depth imaging optical coherence tomography study. Acta Ophthalmol. 2016 Feb;94(1):e68-75. doi: 10.1111/aos.12809. Epub 2015 Aug 13. PMID: 26268377.
3. Brown GL, Camacci ML, Kim SD, Grillo S, Nguyen JV, Brown DA, Ullah SP, Lewis MM, Du G, Kong L, Sundstrom JM, Huang X, Bowie EM. Choroidal Thickness Correlates with Clinical and Imaging Metrics of Parkinson’s Disease: A Pilot Study. J Parkinsons Dis. 2021;11(4):1857-1868. doi: 10.3233/JPD-212676. PMID: 34275909; PMCID: PMC8530855.
4. Kamata Y, Hara N, Satou T, Niida T, Mukuno K. Investigation of the pathophysiology of the retina and choroid in Parkinson’s disease by optical coherence tomography. Int Ophthalmol. 2022 May;42(5):1437-1445. doi: 10.1007/s10792-021-02133-0. Epub 2021 Dec 2. PMID: 34859311; PMCID: PMC9122847.
To cite this abstract in AMA style:
P. Mailankody, R. Battu, PM. Pm, T. K, N. Kamble, R. Yadav, P. Pal. Choroidal changes in Parkinson’s disease: A longitudinal follow up study [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/choroidal-changes-in-parkinsons-disease-a-longitudinal-follow-up-study/. Accessed February 19, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/choroidal-changes-in-parkinsons-disease-a-longitudinal-follow-up-study/