Category: Parkinsonism, Others
Objective: To report the presentation features in autoimmune parkinsonism in a neurological reference center in Arequipa Peru.
Background: Epidemiological studies suggest that a rare association between Parkinsonism and autoimmune diseases exists[1]. Clinical features of parkinsonism become a constituent or a clear manifestation in many autoimmune disorders such as RA, SLE, celiac disease, Sjogren syndrome, among others [2]. The anatomical substrate may involve damage in brainstem and basal ganglia and the later stages of encephalitis and paraneoplastic disease [2]. Many autoantibodies have been associated with parkinsonism pathophysiology; these include anti-GAD (MSA or PSP), VGKC (against LGI1 and CASPR2) as we have previously reported [3], and many others like anti-NMADR (autoimmune encephalitis), anti-DPPX (stiff person syndrome, tremor), anti-Ma2 (onconeural antibodies affecting basal ganglia or upper midbrain) [2]. Even in paraneoplastic disease like B-cell dyscrasias, anti-CV2/CRMP5 in lung cancer, or anti-Ri in opsoclonus myoclonus. [4]
Method: 2650 medical records from a neurological reference center were revised for the terms rigidity, spasticity, tremor, parkinsonism, PSP, MSA, stiff person syndrome, and a matching positive antibody recorded in the medical record. Patients with atypical parkinsonism and positive antibodies were identified retrospectively.
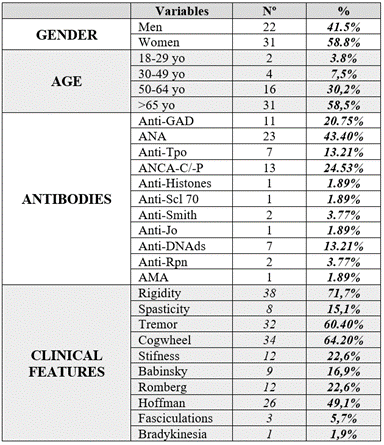
Results: Only 53 records fulfilled the inclusion criteria. [Table 1] Age ranged from 20 to 88 years, with an average of 65.69 years, with more females (58.5%) than males (41.5%). The most common clinical features were: rigidity (71.7%), tremor (60,4%) and spasticity (15.1%). Physical examination showed cogwheel rigidity (64,2%), tremor (60,4%), Hoffman’s (49,1%), Romberg’s (22,6%), stiffness (22,6%), Babinski’s (16,9%), fasciculations(5,7%) and bradykinesia(1,9%). Laboratory findings demonstrated ANA (43.4%), ANCA (24.5%), Anti-GAD (20.8%), Anti-TPO (13.2%), Anti-DNAds (13.2%), Anti-Sm (3.8%), Anti-RNP (3.8%), Anti-histones, Anti-Scl 70 , Anti-Jo , and AMA (1.9% each). With some of the patients presenting with more than one antibody. All patients were treated with antiparkinsonism drugs and immunomodulatory therapy and 69.9% of patients improved.
Conclusion: This case series raises the role of neuroinflammation in parkinsonism, however nonsuch one exclusive pathophysiologic pathway could be made solely responsible, although in most cases immune therapy improved the symptoms [1].
Table 1. Characteristics of the Sample
References: 1. Kannoth S et al. Autoimmune atypical parkinsonism — A group of treatable parkinsonism. Journal of the Neurological Sciences 2016;3620(40-46). Available from: https://www.jns-journal.com/article/ S0022-510X(16)30008-9/abstract
2. Barba C, Alexopoulos H. Parkinsonism in autoimmune diseases. International Review of Neurobiology. 2019;419–52.
3. Trillo W et al. Sporadic Creutzfeldt-Jakob disease mimic due to voltage gated potassium channel antibodies (VGKC) autoimmune encephalitis. (case report). Journal of the Neurological Sciences 2019;405(91). Available from: https://www.jns-journal.com/article/S0022-510X(19)31416-9/fulltext#relatedArticles
4. Gövert F, Leypoldt F, Junker R, Wandinger K-P, Deuschl G, Bhatia KP, et al. Antibody-related movement disorders – a comprehensive review of phenotype-autoantibody correlations and a guide to testing. Neurological Research and Practice. 2020 Feb 20;2(1).
To cite this abstract in AMA style:
W. Trillo Alvarez, C. Ibañez Escalante, A. Escalante Mercado, P. Bermejo Rosado, L. Delgado Villanueva, A. Aquino Toledo, R. Huanca Machon. Characterization of Autoimmune Parkinsonism. A case series [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/characterization-of-autoimmune-parkinsonism-a-case-series/. Accessed April 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/characterization-of-autoimmune-parkinsonism-a-case-series/