Session Information
Date: Tuesday, September 24, 2019
Session Title: Neurophysiology
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To investigate the properties of central and peripheral innervation in Parkinson disease (PD) using transcranial magnetic stimulation (TMS) and electroneurography (ENG), also to evaluate the impact of PD on the quality of life (QOL).
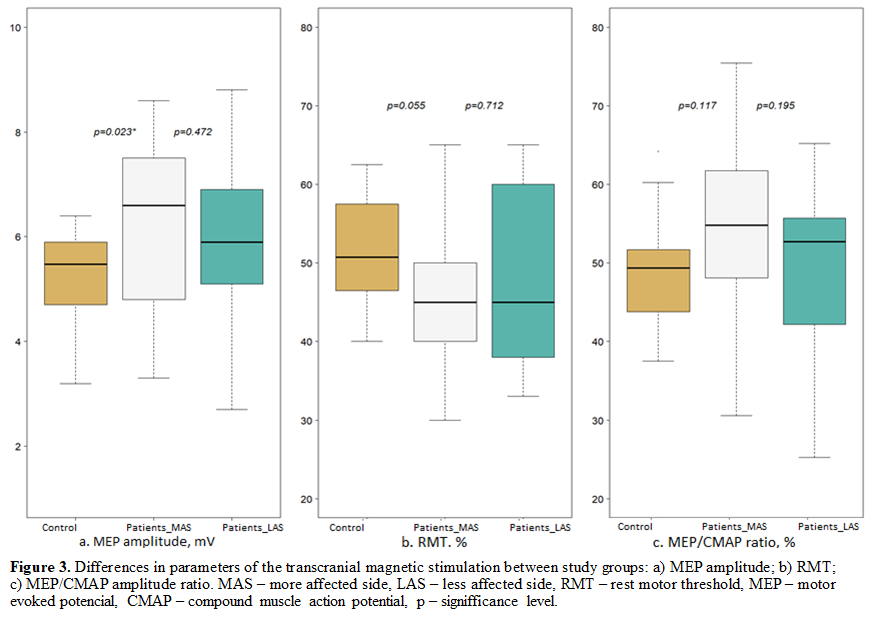
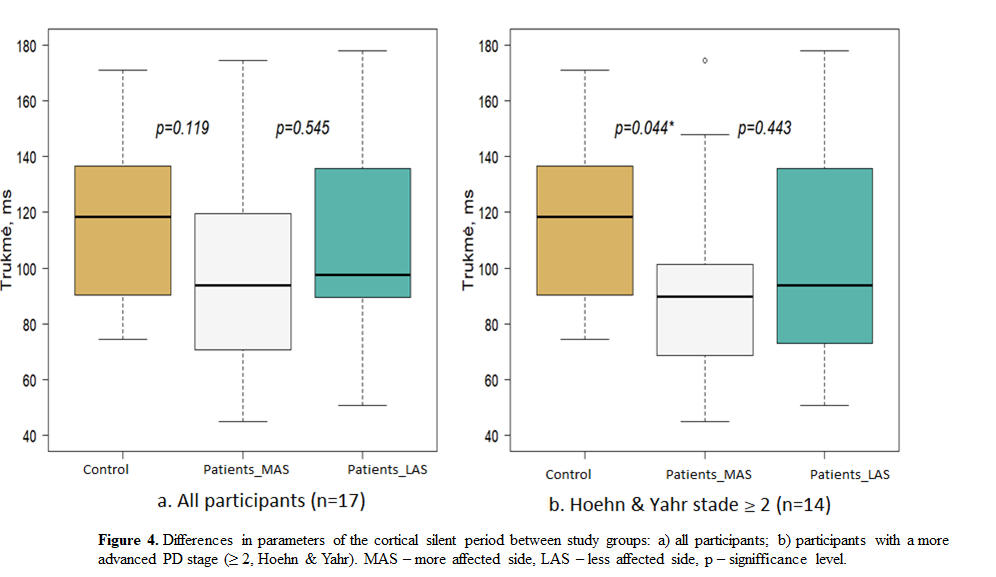
Background: One of the approaches to explaining Parkinson’s disease (PD) pathophysiology is an impaired control of the agonist-antagonist muscle groups, linked to disrupted internal central nervous system (CNS) networks. Transcranial magnetic stimulation (TMS) is a useful tool to study functional connections in the human brain. CSP is obtained upon stimulation of the contralateral motor cortex during maximal muscle contraction and is one of the parameters of intracortical inhibition. Shortening of this parameter during the course of PD can be interpreted as a reflection of the disruption of neuronal networks. CuSP reflects the action of inhibitory networks at the spinal level and is obtained while stimulating the thin peripheral nerve fibers during maximal voluntary muscle contraction. CuSP is elongated in early PD and shortened with the progression of the disease – might reflect a compensatory mechanism for altered movement control in the cerebral cortex.
Method: Participants underwent neurological examination, including UPDRS III scale (PD patients) and responded to SF-36 questionnaire. Neurophysiological studies were performed bilaterally on the ulnar nerve and abductor digiti minimi muscle, using Nicolet Viking and Magstim 200 electrodiagnostic system.
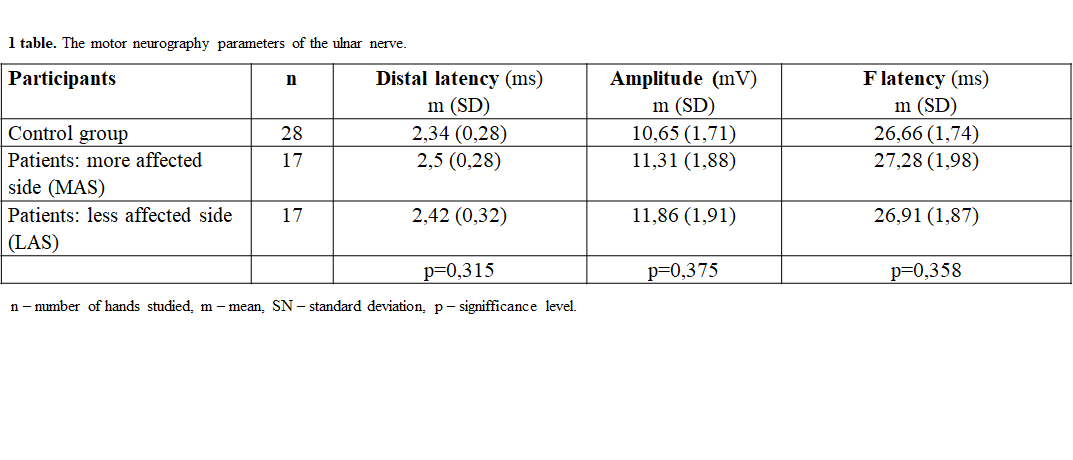
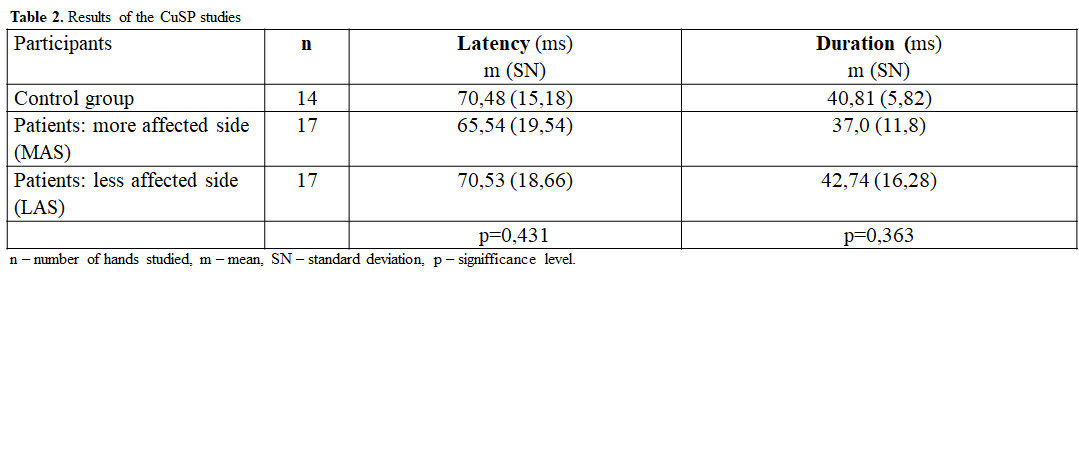
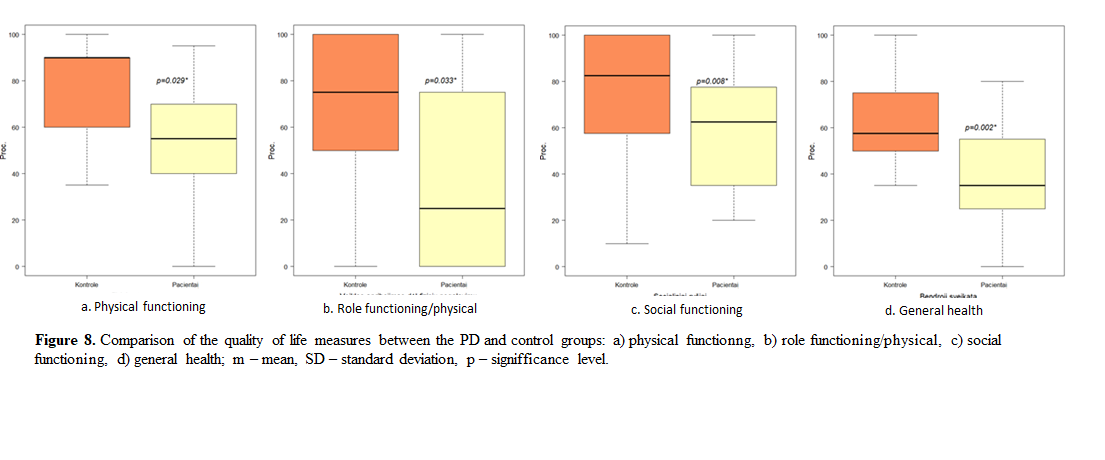
Results: 17 PD patients and 14 healthy controls participated in the study. Peripheral nerve conduction was in the normal range in both groups (table 1). CuSP measures were similar in both groups, but greater standard deviation was observed in the PD group (table 2). CSP was shorter in the more affected side (MAS) of the PD group (figure 1) and that difference was statistically significant in patients with a more advanced PD stage (p=0,0439) (figure 2). QOL in the PD group was significantly worse in 4 of 8 scores of the SF-36 questionnaire (figure 3).
Conclusion: Impairment of inhibitory networks can be considered as a pathophysiological mechanism in PD. Further studies are needed to evaluate the impact of clinical variables on the measures of neurophysiological tests, also to establish a common mechanism affecting the duration of both CuSP and CSP. PD had a significant effect on the patients‘ QOL.
To cite this abstract in AMA style:
L. Sinkunaite, J. Svilpauske-Lauryniene, D. Garsviene, D. Surkiene. Changes of cutaneous and cortical silent responses in a random sample of Lithuania patients with Parkinson disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/changes-of-cutaneous-and-cortical-silent-responses-in-a-random-sample-of-lithuania-patients-with-parkinson-disease/. Accessed December 14, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/changes-of-cutaneous-and-cortical-silent-responses-in-a-random-sample-of-lithuania-patients-with-parkinson-disease/