Category: Rating Scales
Objective: To provide a comprehensive review of various patient-reported outcome (PROs) used in movement disorders (MD) research and their MCID values reported in literature.
Background: There is a growing awareness of significance of using MCID in MD research. MCID is the smallest change in an outcome measure that is considered clinically meaningful. MCID can ensure trials are adequately powered to detect meaningful treatment effects, aid in interpretation of treatment outcomes, and development of new outcome measures, and aid in selection of appropriate endpoints.[1],[2],[3]
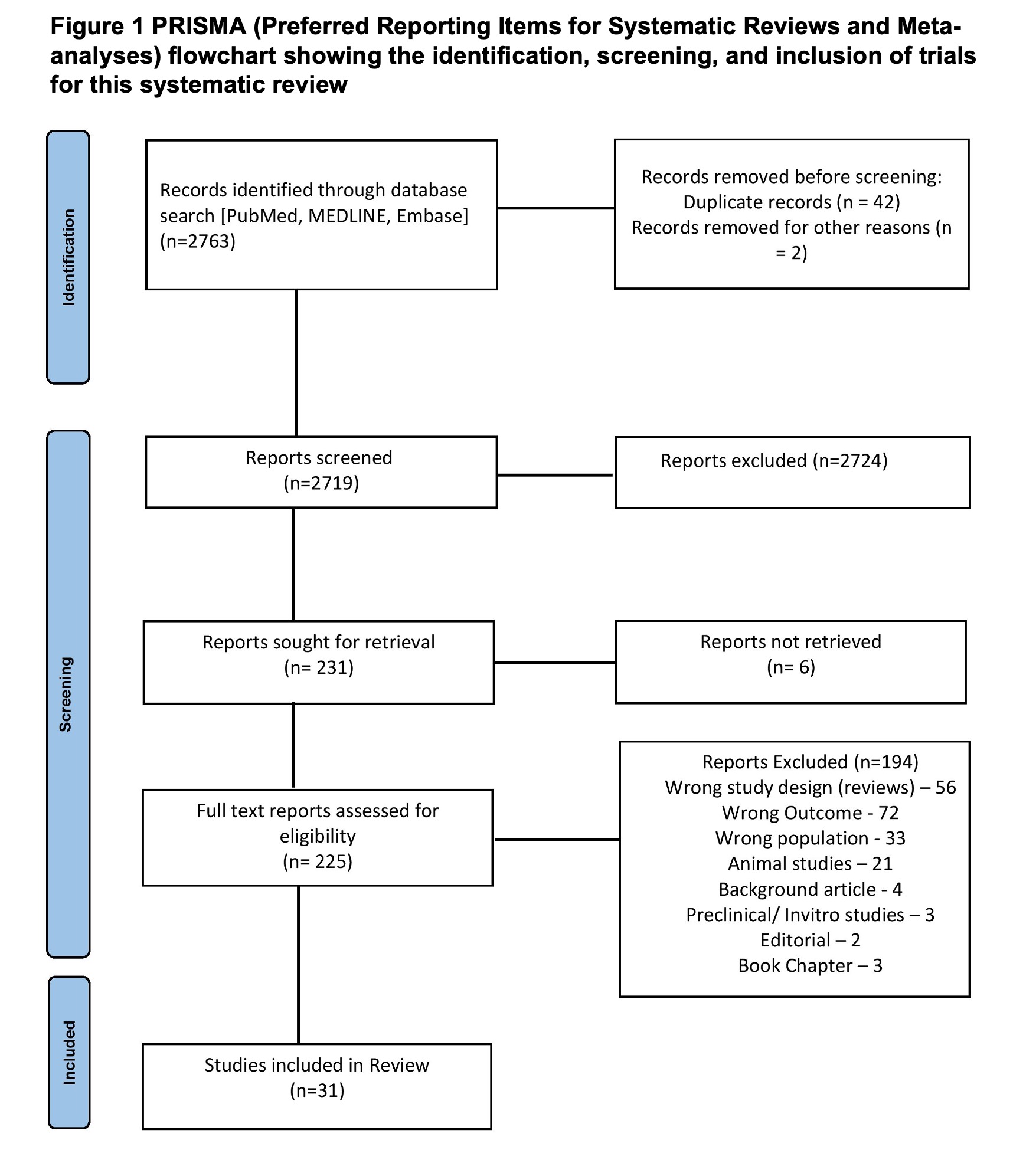
Method: Inclusion criteria:(a) studies published in English,(b) studies reporting MCID scales, and(c) studies reporting on one or more movement disorders, including Parkinsonism, Dystonia, tremor, tics, dyskinesia, tardive, or chorea. Databases searched included PubMed, Embase and MEDLINE.
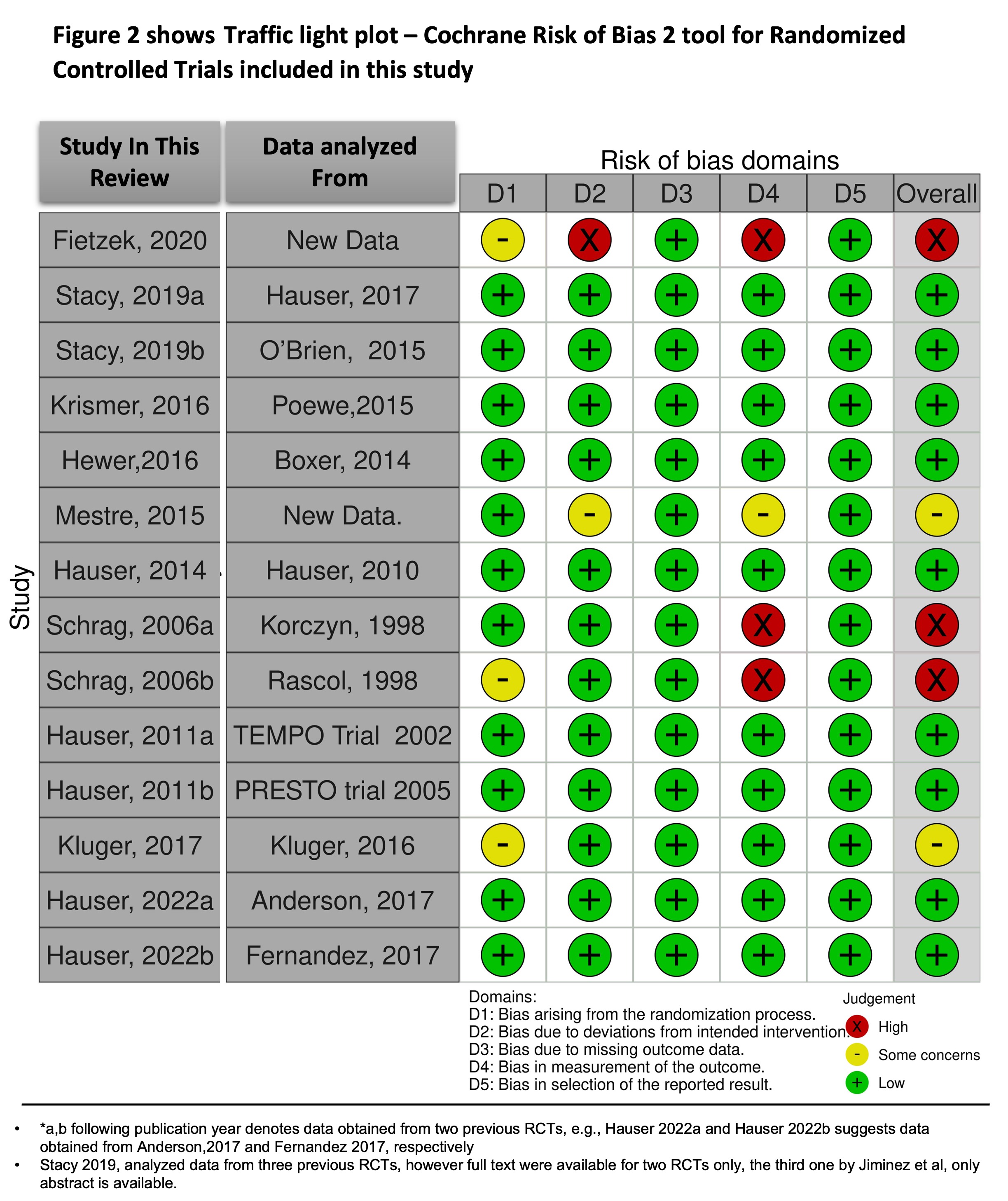
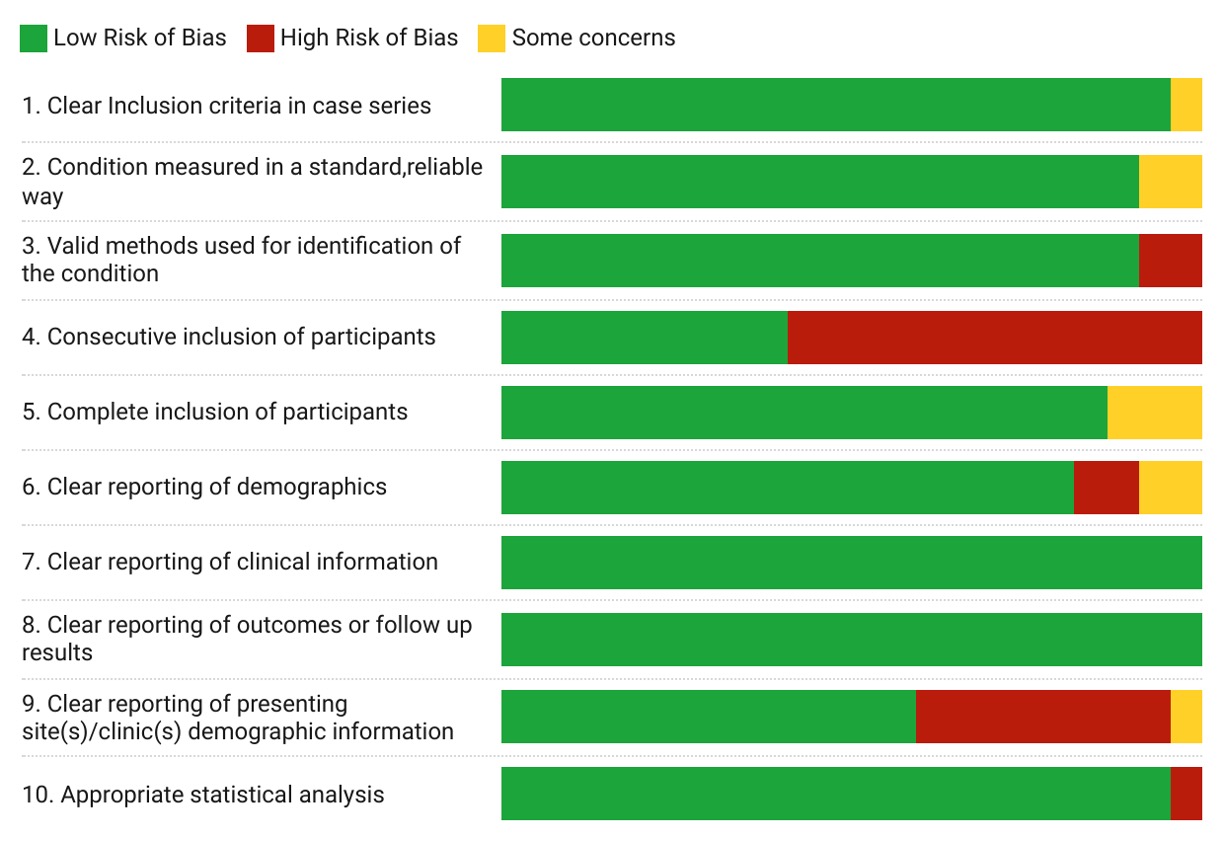
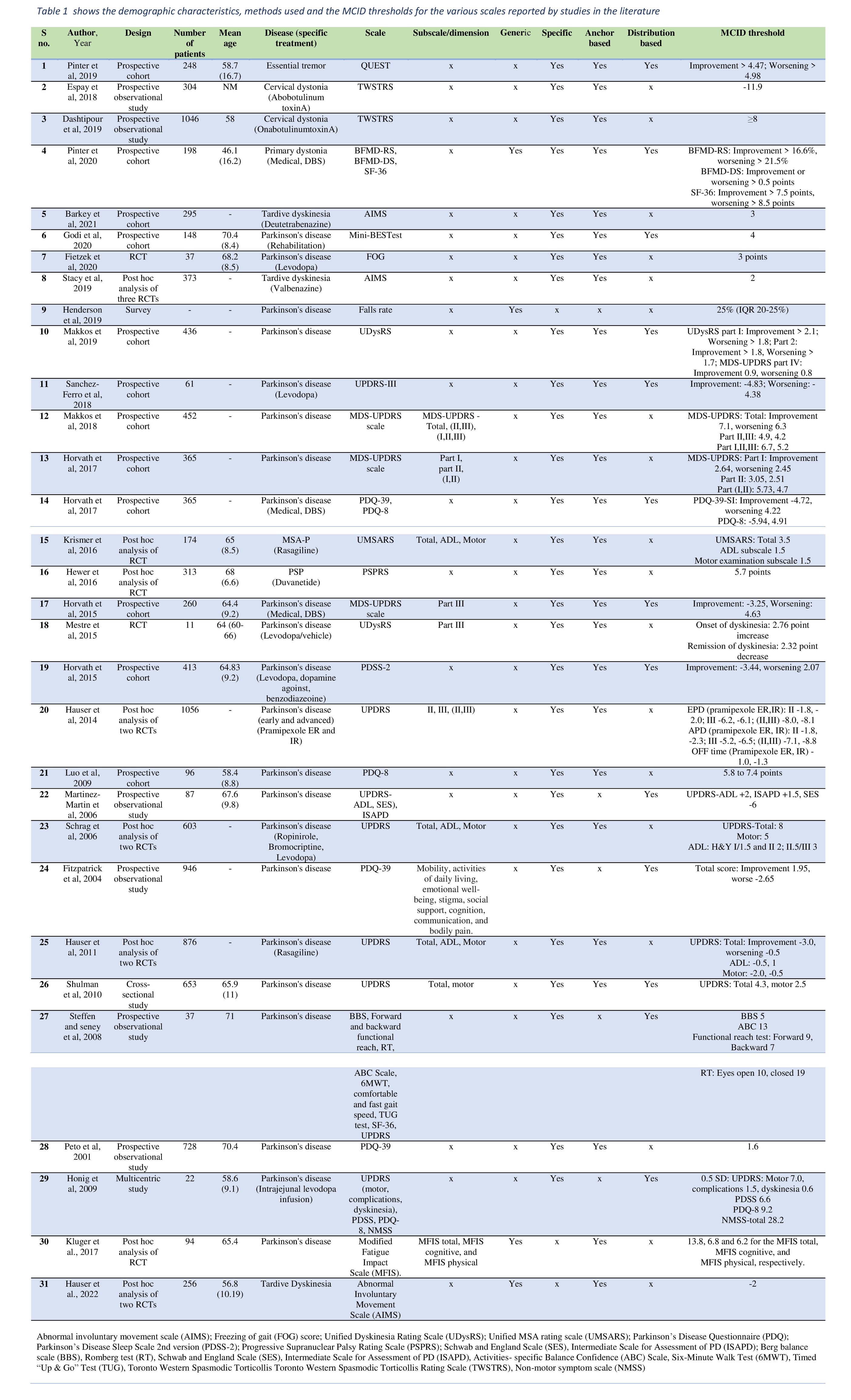
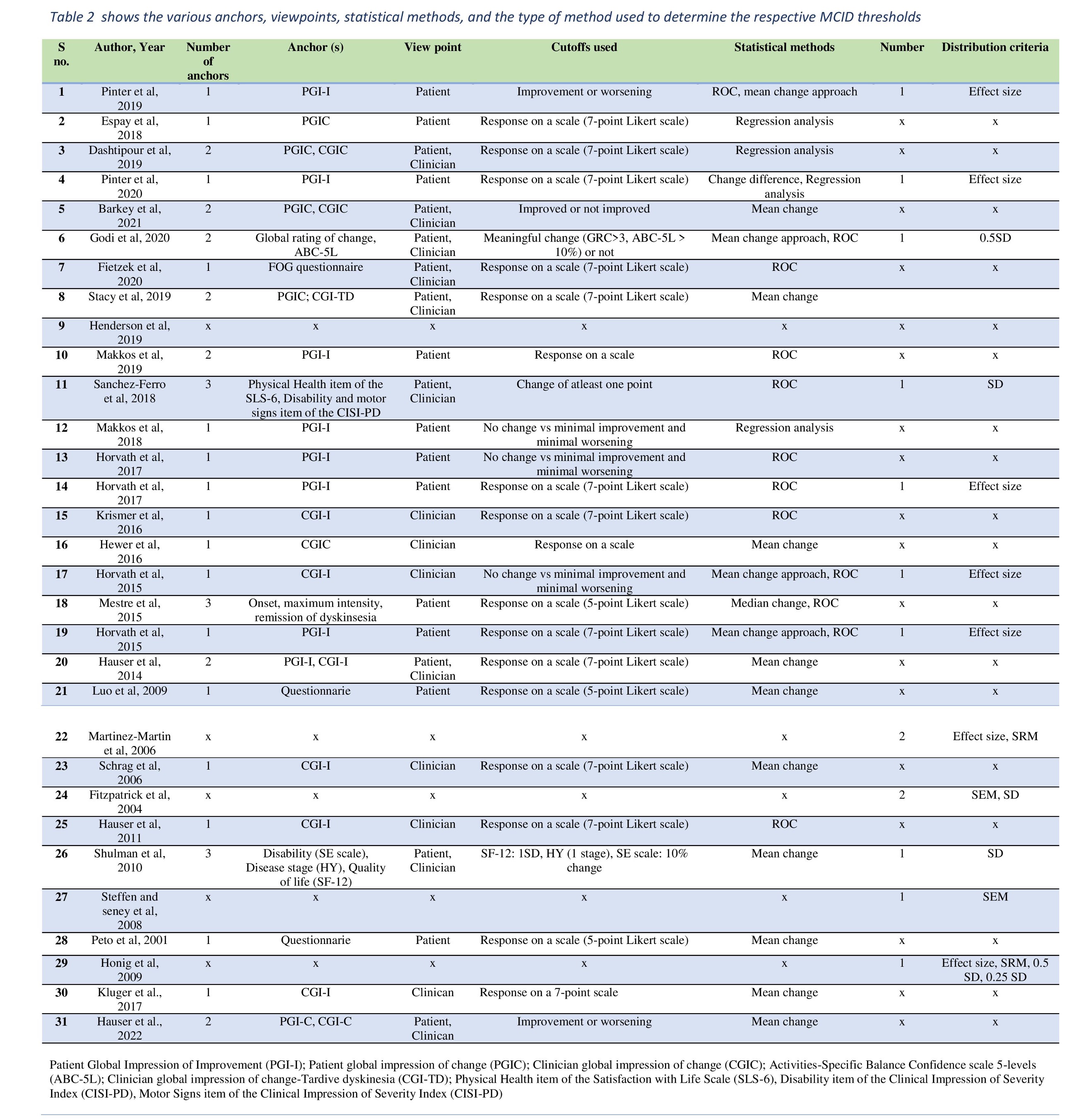
Results: Final review included 31 studies[Figure1]. Among the 10 RCTs included, majority(n=6) had low risk of bias (RoB),2 had high RoB and 2 had some concerns.[4][5][Figure2] Among the remaining non-RCTs, majority showed low RoB in all domains of JBI tool, except for domain of consecutive enrolment of patients (domain no. 4 ) and site of study (domain no.9).[6][Figure3] Overall the included studies were of good quality. There was considerable variability in the MD studied as well as the scales used. MCID values were most commonly reported for UPDRS scale (n=11, MCID ranging from 1.8 to 8 points for various subsections of UPDRS for improvement (IMP) and from 2 to 10.7 points for worsening(WOR)). 3 studies each reported on AIMS (MCID 2-3 points), PDQ 39 (MCID IMP 1.6 to 4.7; WOR 2.6 to 4.2 points), PDQ 8 ( MCID IMP 5.9 to 9.2; WOR 4.9 to 7.4 points), and UDysRS (MCID: IMP >1.8 to 2.1; WOR >1.8 to >1.7).[Table1,2][7-37]
Conclusion: The review is significant in that it combines all MCID scales currently reported in MD patients, for the first time in literature, providing a comprehensive resource for future trials. This review highlights the need for standardized and validated MCID scales in MD research to help clinicians and researchers interpret study results and to make informed decisions about patient care. MCID scales can also help to ensure that future MD trials are designed and conducted in a way that is most meaningful and relevant to patients.
References: [1] Stang A, Poole C, Kuss O. The ongoing tyranny of statistical significance testing in biomedical research. Eur J Epidemiol. 2010 Apr;25(4):225–30.
[2] Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J Off J North Am Spine Soc. 2007 Oct;7(5):541–6.
[3] Draak THP, de Greef BTA, Faber CG, Merkies ISJ, PeriNomS study group. The minimum clinically important difference: which direction to take. Eur J Neurol. 2019 Jun;26(6):850–5.
[4] RoB 2: a revised tool for assessing risk of bias in randomised trials | The BMJ. https://www.bmj.com/content/366/bmj.l4898 (accessed Oct 28, 2022).
[5] McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods [Internet]. 2020 Apr 26 [cited 2020 May 21];n/a(n/a). Available from: https://doi.org/10.1002/jrsm.1411
[6] Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18:2127–2133. doi:10.11124/ JBISRIR-D-19-00099.
[7] Pintér D, Makkos A, Kovács M, Janszky J, Kovács N. Minimal clinically important difference for the quality of life in essential tremor questionnaire. Mov Disord Off J Mov Disord Soc. 2019 May;34(5):759–60.
[8] Hewer S, Varley S, Boxer AL, Paul E, Williams DR, AL-108-231 Investigators. Minimal clinically important worsening on the progressive supranuclear Palsy Rating Scale. Mov Disord Off J Mov Disord Soc. 2016 Oct;31(10):1574–7.
[9] Barkay H, Hauser RA, Wilhelm A, Wieman M, Gordon MF, Savola JM. Minimal Clinically Important Difference in AIMS Score Based on CGIC and PGIC in Patients With Tardive Dyskinesia Treated With Deutetrabenazine. CNS Spectr. 2021 Apr;26(2):159.
[10] Fietzek UM, Schulz SJ, Ziegler K, Ceballos-Baumann AO. The Minimal Clinically Relevant Change of the FOG Score. J Park Dis. 2020;10(1):325–32.
[11] Fitzpatrick R, Norquist JM, Jenkinson C. Distribution-based criteria for change in health-related quality of life in Parkinson’s disease. J Clin Epidemiol. 2004 Jan;57(1):40–4.
[12] Godi M, Arcolin I, Giardini M, Corna S, Schieppati M. Responsiveness and minimal clinically important difference of the Mini-BESTest in patients with Parkinson’s disease. Gait Posture. 2020 Jul;80:14–9.
[13] Dashtipour K, Mari Z, Jankovic J, Adler CH, Schwartz M, Brin MF. Minimal clinically important change in patients with cervical dystonia: Results from the CD PROBE study. J Neurol Sci. 2019 Oct 15;405:116413.
[14] Espay AJ, Trosch R, Suarez G, Johnson J, Marchese D, Comella C. Minimal clinically important change in the Toronto Western Spasmodic Torticollis Rating Scale. Parkinsonism Relat Disord. 2018 Jul;52:94–7.
[15] Hauser RA, Barkay H, Wilhelm A, Wieman M, Savola JM, Gordon MF. Minimal clinically important change in Abnormal Involuntary Movement Scale score in tardive dyskinesia as assessed in pivotal trials of deutetrabenazine. Parkinsonism Relat Disord. 2022 Apr 1;97:47–51.
[16] Pintér D, Janszky J, Kovács N. Minimal Clinically Important Differences for Burke-Fahn-Marsden Dystonia Rating Scale and 36-Item Short-Form Health Survey. Mov Disord Off J Mov Disord Soc. 2020 Jul;35(7):1218–23.
[17] Hauser RA, Auinger P, Parkinson Study Group. Determination of minimal clinically important change in early and advanced Parkinson’s disease. Mov Disord Off J Mov Disord Soc. 2011 Apr;26(5):813–8.
[18] Hauser RA, Gordon MF, Mizuno Y, Poewe W, Barone P, Schapira AH, et al. Minimal clinically important difference in Parkinson’s disease as assessed in pivotal trials of pramipexole extended release. Park Dis. 2014;2014:467131.
[19] Henderson EJ, Morgan GS, Amin J, Gaunt DM, Ben-Shlomo Y. The minimum clinically important difference (MCID) for a falls intervention in Parkinson’s: A delphi study. Parkinsonism Relat Disord. 2019 Apr;61:106–10.
[20] Honig H, Antonini A, Martinez-Martin P, Forgacs I, Faye GC, Fox T, et al. Intrajejunal levodopa infusion in Parkinson’s disease: a pilot multicenter study of effects on nonmotor symptoms and quality of life. Mov Disord Off J Mov Disord Soc. 2009 Jul 30;24(10):1468–74.
[21] Horváth K, Aschermann Z, Ács P, Deli G, Janszky J, Komoly S, et al. Minimal Clinically Important Difference on Parkinson’s Disease Sleep Scale 2nd Version. Park Dis. 2015;2015:970534.
[22] Horváth K, Aschermann Z, Ács P, Deli G, Janszky J, Komoly S, et al. Minimal clinically important difference on the Motor Examination part of MDS-UPDRS. Parkinsonism Relat Disord. 2015 Dec;21(12):1421–6.
[23] Horváth K, Aschermann Z, Kovács M, Makkos A, Harmat M, Janszky J, et al. Changes in Quality of Life in Parkinson’s Disease: How Large Must They Be to Be Relevant? Neuroepidemiology. 2017;48(1–2):1–8.
[24] Horváth K, Aschermann Z, Kovács M, Makkos A, Harmat M, Janszky J, et al. Minimal clinically important differences for the experiences of daily living parts of movement disorder society-sponsored unified Parkinson’s disease rating scale. Mov Disord Off J Mov Disord Soc. 2017 May;32(5):789–93.
[25] Kluger BM, Garimella S, Garvan C. Minimal clinically important difference of the Modified Fatigue Impact Scale in Parkinson’s disease. Parkinsonism Relat Disord. 2017 Oct;43:101–4.
[26] Krismer F, Seppi K, Wenning GK, Abler V, Papapetropoulos S, Poewe W. Minimally clinically important decline in the parkinsonian variant of multiple system atrophy. Mov Disord Off J Mov Disord Soc. 2016 Oct;31(10):1577–81.
[27] Luo N, Tan LCS, Zhao Y, Lau PN, Au WL, Li SC. Determination of the longitudinal validity and minimally important difference of the 8-item Parkinson’s Disease Questionnaire (PDQ-8). Mov Disord Off J Mov Disord Soc. 2009 Jan 30;24(2):183–7.
[28] Makkos A, Kovács M, Aschermann Z, Harmat M, Janszky J, Karádi K, et al. Are the MDS-UPDRS-Based Composite Scores Clinically Applicable? Mov Disord Off J Mov Disord Soc. 2018 May;33(5):835–9.
[29] Makkos A, Kovács M, Pintér D, Janszky J, Kovács N. Minimal clinically important difference for the historic parts of the Unified Dyskinesia Rating Scale. Parkinsonism Relat Disord. 2019 Jan;58:79–82.
[30] Martinez-Martin P, Prieto L, Forjaz MJ. Longitudinal metric properties of disability rating scales for Parkinson’s disease. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2006 Dec;9(6):386–93.
[31] Mestre TA, Beaulieu-Boire I, Aquino CC, Phielipp N, Poon YY, Lui JP, et al. What is a clinically important change in the Unified Dyskinesia Rating Scale in Parkinson’s disease? Parkinsonism Relat Disord. 2015 Nov;21(11):1349–54.
[32] Peto V, Jenkinson C, Fitzpatrick R. Determining minimally important differences for the PDQ-39 Parkinson’s disease questionnaire. Age Ageing. 2001 Jul;30(4):299–302.
[33] Sánchez-Ferro Á, Matarazzo M, Martínez-Martín P, Martínez-Ávila JC, Gómez de la Cámara A, Giancardo L, et al. Minimal Clinically Important Difference for UPDRS-III in Daily Practice. Mov Disord Clin Pract. 2018 Aug;5(4):448–50.
[34] Schrag A, Sampaio C, Counsell N, Poewe W. Minimal clinically important change on the unified Parkinson’s disease rating scale. Mov Disord Off J Mov Disord Soc. 2006 Aug;21(8):1200–7.
[35] Shulman LM, Gruber-Baldini AL, Anderson KE, Fishman PS, Reich SG, Weiner WJ. The clinically important difference on the unified Parkinson’s disease rating scale. Arch Neurol. 2010 Jan;67(1):64–70.
[36] Stacy M, Sajatovic M, Kane JM, Cutler AJ, Liang GS, O’Brien CF, et al. Abnormal involuntary movement scale in tardive dyskinesia: Minimal clinically important difference. Mov Disord Off J Mov Disord Soc. 2019 Aug;34(8):1203–9.
[37] Steffen T, Seney M. Test-retest reliability and minimal detectable change on balance and ambulation tests, the 36-item short-form health survey, and the unified Parkinson disease rating scale in people with parkinsonism. Phys Ther. 2008 Jun;88(6):733–46.
To cite this abstract in AMA style:
B. Mishra, S. Pachipala, R. Rajan, A. Agarwal, MVP. Srivastava, N. Nilima, VY. Vishnu. Bridging the Gap between Statistical significance and Clinical Relevance: A Systematic Review of Minimum clinically important difference (MCID) thresholds of scales reported in trials of Movement Disorders [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/bridging-the-gap-between-statistical-significance-and-clinical-relevance-a-systematic-review-of-minimum-clinically-important-difference-mcid-thresholds-of-scales-reported-in-trials-of-movement-diso/. Accessed December 30, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/bridging-the-gap-between-statistical-significance-and-clinical-relevance-a-systematic-review-of-minimum-clinically-important-difference-mcid-thresholds-of-scales-reported-in-trials-of-movement-diso/