Objective: To assess whether including measurements of neuroimaging and biofluid-based biomarkers improves predictive ability of models of motor and non-motor progression up to 5-year follow-up in early Parkinson’s Disease (PD).
Background: Currently, diagnosis of PD remains challenging, with a low reported diagnostic accuracy in early PD [1]. Multimodal models, incorporating biomarker measurement, may more accurately predict disease progression compared to clinical symptom presentation alone.
Method: Data from the Parkinson’s Progression Markers Initiative (PPMI) study were used. As a proxy of substantia nigra (SN) volume, we manually masked the SN-related T2-hypointensity. Hierarchical and fuzzy C-means clustering analyses were performed on motor and cognitive/mood outcomes, respectively, at five-year follow-up. The ability of baseline clinical, neuroimaging (proxy SN volume/DaT binding) and biofluid markers (alpha-syn/p-tau/amyloid beta/IGF-1) to predict cluster membership at five-year follow-up was assessed using logistic (motor) or linear (cognitive/mood) regression.
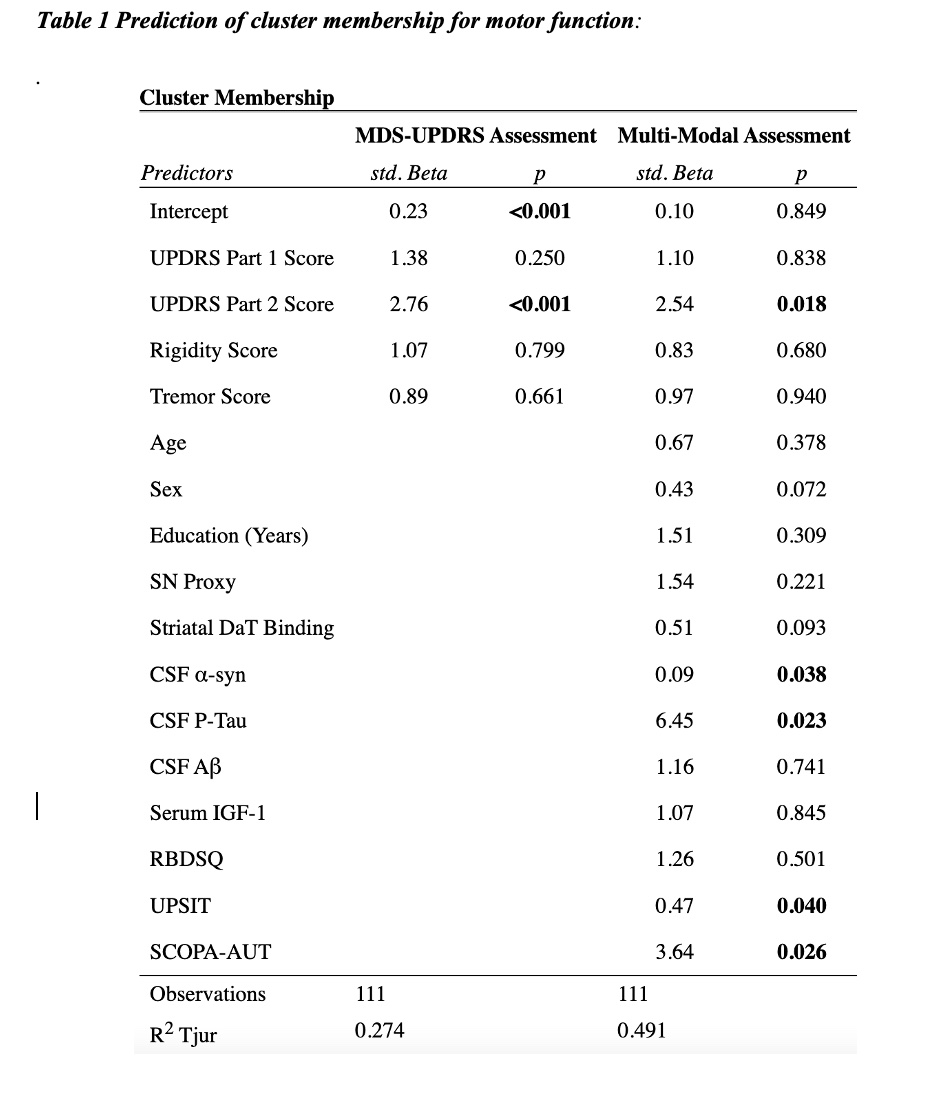
Results: Two clusters were defined in the motor analysis (n= 300), with higher rigidity and impaired cognitive/motor/mood function at 5-year follow-up in the first cluster, compared to the second more tremor-dominant cluster. Cluster membership was predicted by UPDRS Part 2 score, CSF levels of alpha synuclein and hyperphosphorylated tau (pTau) and prodromal symptom presentation at baseline (Table 1). This multimodal model accounted for 49.1% of the variance, compared to 27.4% in the model including UPDRS score alone.
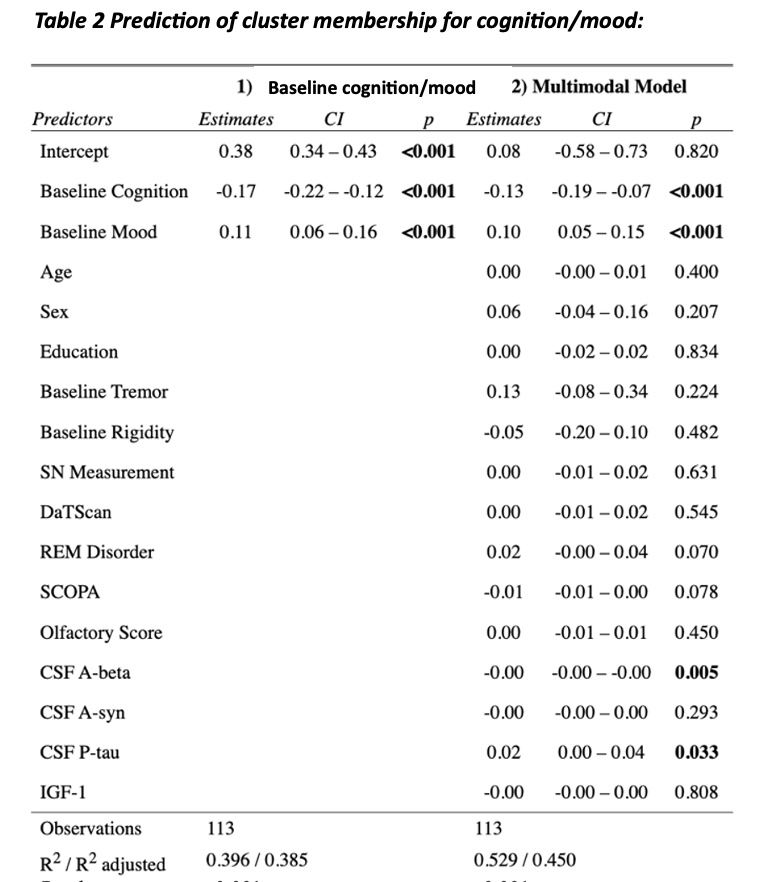
For cognition/mood (n = 309), two clusters were defined, with older age, worsened cognitive/motor/mood function, increased prodromal symptom presentation, lower striatal DaT binding and reduced CSF levels of amyloid-beta (Ab) in the second cluster. Membership in this cluster was predicted by baseline mood and cognition scores and CSF levels of both Ab and pTau, with the model accounting for 52.9% of the variance, compared to 39.6% in the model including baseline cognition/mood alone (Table 2).
Conclusion: Multimodal models, including both clinical and objective biomarker measures, have potential utility for improving prediction of both motor and non-motor symptom progression at five-year follow-up. Understanding disease progression in PD is critical for disease management and therapeutic development.
Table 1: Cluster membership prediction for motor
Table 2: Cluster prediction for cognition/mood
References: [1] Beach TG and Adler CH. Importance of low diagnostic accuracy for early Parkinson’s disease. Mov Disord. 2018; 33(10): 1551-1554.
To cite this abstract in AMA style:
L. Collins-Praino, A. Mcnamara, B. Ellul, I. Baetu, S. Lau, M. Jenkinson. Beyond Clinical Presentation: Incorporating Neuroimaging and Biofluid Markers to Predict Progression of Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/beyond-clinical-presentation-incorporating-neuroimaging-and-biofluid-markers-to-predict-progression-of-parkinsons-disease/. Accessed February 19, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/beyond-clinical-presentation-incorporating-neuroimaging-and-biofluid-markers-to-predict-progression-of-parkinsons-disease/