Category: Parkinson's Disease: Neuroimaging
Objective: In the current study, we aimed to examine structural MRI data from a large sample of de novo PD patients and to identify potential biomarker(s) to predict the onset of dyskinesias in them.
Background: Levodopa-induced dyskinesia is a major complication that disables a large percentage of patients with Parkinson’s disease (PD). The small sample sizes of clinical and neuroimaging studies and the dearth of longitudinal patient data prior to starting treatment make it difficult to predict the susceptibility of PD patients to develop dyskinesias.
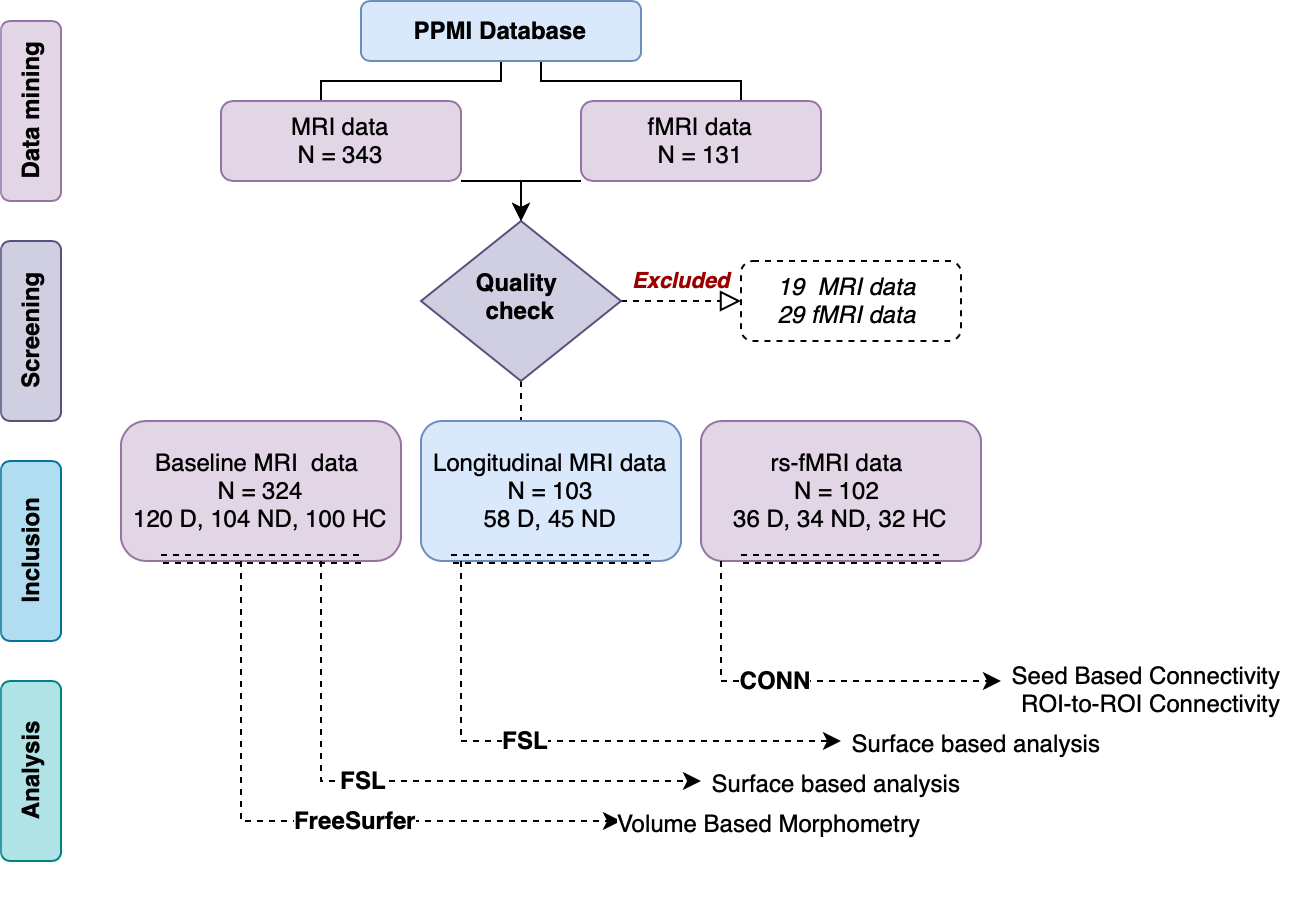
Method: We curated MRI data of 120 dyskinetic, 104 non-dyskinetic PD patients from the Parkinson’s Progression Markers Initiative (PPMI) database and compared them with data from 100 age and gender-matched healthy controls. We examined the volume and shape changes in cortical as well as subcortical structures across the 3 subject groups. Further, we also examined resting-state functional connectivity and longitudinal progression of structural changes in a subset of these patients.
Results: Volumetric analysis did not reveal significant differences between dyskinetic and non-dyskinetic groups. However, we found significantly larger left fusiform and left posterior cingulate gyrus in dyskinetics than in healthy controls. While dyskinetics showed no significant changes in basal ganglia volume, bilateral putaminal volumes were significantly lower in non-dyskinetics compared to healthy controls. Vertex-based shape analysis revealed a local increase in the surface area of the left caudate, left putamen and a global increase in the left pallidum in dyskinetics alone. Longitudinal analysis revealed a progressive increase in the surface area of the left caudate in dyskinetics. Besides structural differences, we found that the seed-based functional connectivity of the right caudate and left post-central gyrus were significantly different between dyskinetics and non-dyskinetics.
Conclusion: Our findings are suggestive of striatal growth in dyskinetic and atrophy in non-dyskinetic PD patients even prior to starting levodopa therapy. These structural changes are more prominent on the more affected side and progress with disease duration. Histopathological characterisation of the growth in the basal ganglia would be needed to further understand the pathological basis of dyskinesias.
To cite this abstract in AMA style:
S. Shukla, M. Patnaik, A. Kumar, N. Thirugnanasambandam, S. Tinaz. Basal ganglia shape in de novo Parkinson’s disease patients can predict the onset of Levodopa Induced Dyskinesias [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/basal-ganglia-shape-in-de-novo-parkinsons-disease-patients-can-predict-the-onset-of-levodopa-induced-dyskinesias/. Accessed May 10, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/basal-ganglia-shape-in-de-novo-parkinsons-disease-patients-can-predict-the-onset-of-levodopa-induced-dyskinesias/