Category: Parkinson's Disease: Neuroimaging
Objective: In patients with parkinsonism and uncertain differential diagnosis, an automated image-based algorithm can help to distinguish idiopathic Parkinson’s disease (IPD) from atypical parkinsonian syndromes (APS). Here, we evaluated the accuracy of an automated imaging classification for differential diagnosis in parkinsonism in patients that received an autopsy confirmed diagnosis of Parkinson’s disease (PD), multiple system atrophy (MSA), or progressive supranuclear palsy (PSP).
Background: In clinically uncertain cases, accurate discrimination can be achieved with the automated algorithm several years before a final diagnosis is reached by a movement disorder specialist [1,2]. In these studies, image-based classifications accorded well with the ultimate diagnosis of the movement disorders specialist. However, postmortem confirmation representing the diagnostic gold standard for parkinsonian disorders was lacking.
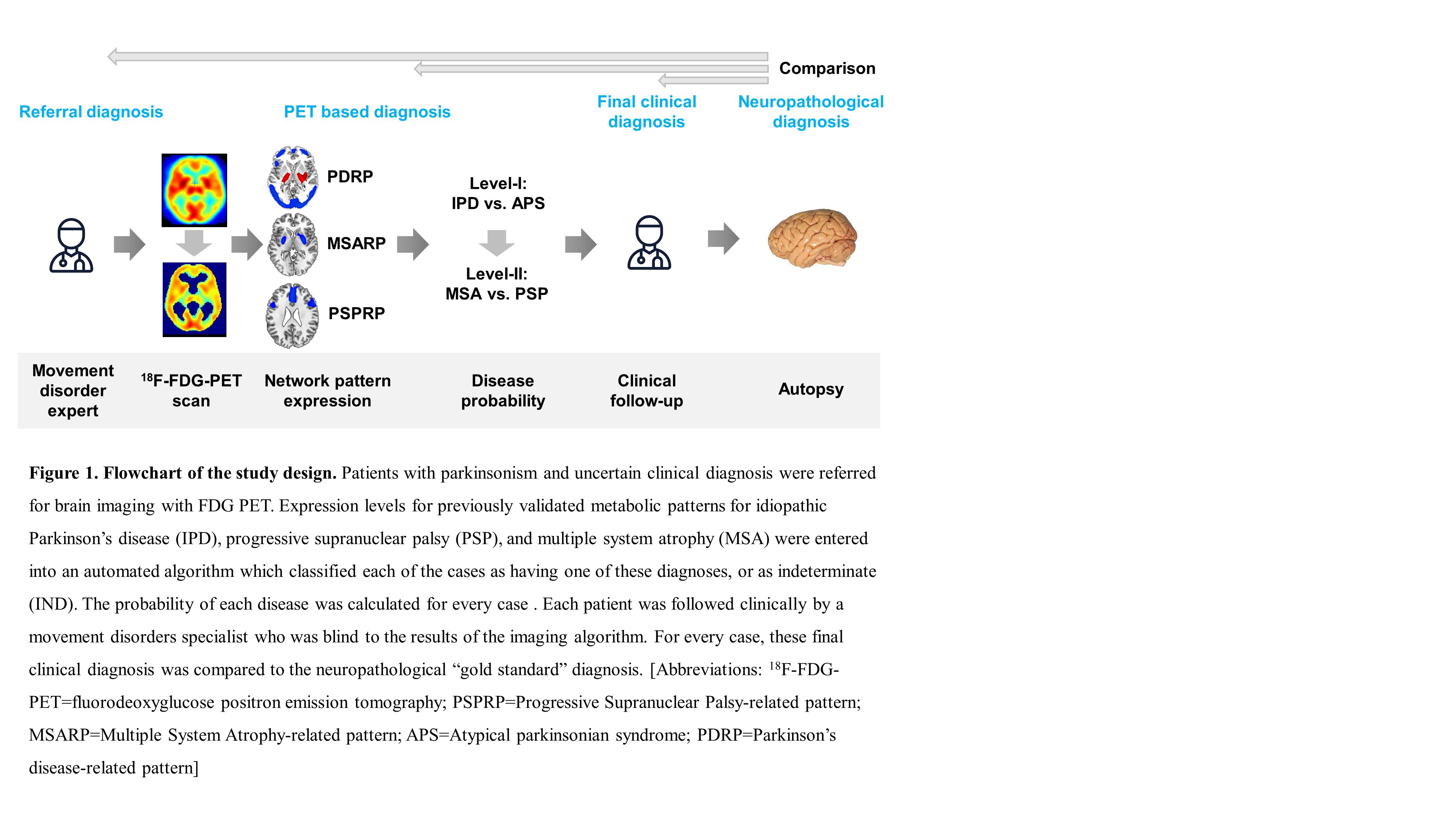
Method: Patients with parkinsonism and uncertain clinical diagnosis were referred for 18F-fluorodeoxyglucose (FDG) PET imaging. Expression levels for previously validated metabolic patterns for PD, MSA, and PSP were entered into an automated algorithm which classified each of the cases. The leading clinical diagnosis at the time of referral was recorded for each patient as well as the final clinical diagnosis of a movement disorders expert, an average of 1.9 years (range 4.4) after imaging [figure 1]. In all cases, both initial and final clinical diagnosis were obtained blind to the imaging results.
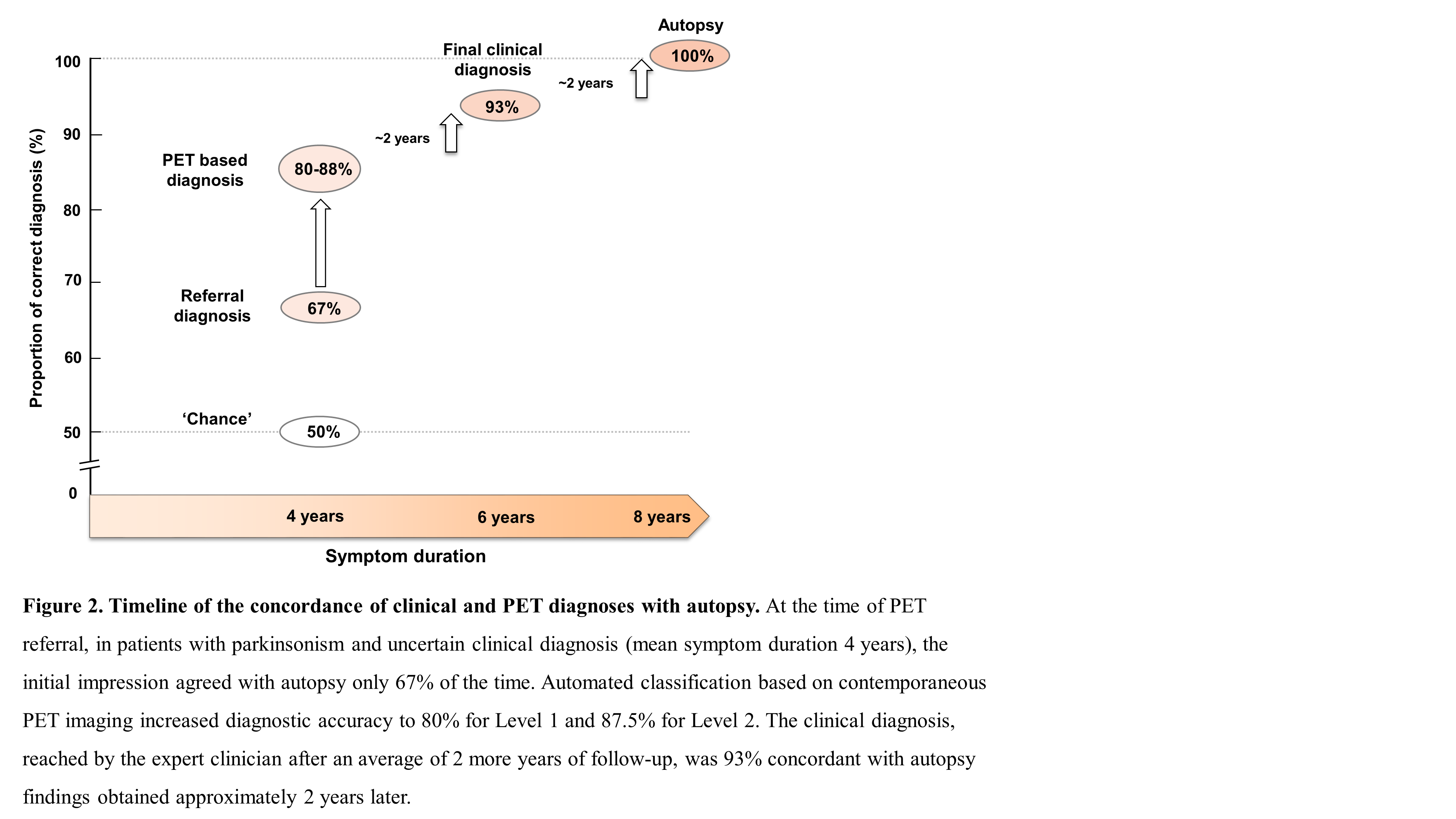
Results: Fifteen of the patients had autopsy an average of 3.5±1.6 years after imaging, with diagnoses of IPD (n=4), MSA (n=6), and PSP (n=5). The mean symptom duration at the time of referral was 4.1±2.6 years. Compared to the autopsy “gold standard”, the classification algorithm correctly identified 80% of the cases as IPD or APS (p=0.01, binomial test; 87.5% of APS cases were correctly identified as MSA or PSP (p=0.02)). The initial referral diagnosis, by contrast, was only 66.7% correct (p=0.1), whereas the final clinical diagnosis (1.9±1.4 years after imaging) was 93.3% accurate (p=0.0004) [figure 2].
Conclusion: At the time of PET referral, the image-based algorithm substantially reduced diagnostic uncertainty relative to the autopsy “gold standard”. While the final clinical diagnosis had nearly perfect concordance with autopsy, this degree of accuracy required several more years of expert follow-up.
References: Tang CC, Poston KL, Eckert T, et al. Differential diagnosis of parkinsonism: a metabolic imaging study using pattern analysis. Lancet Neurol 2010; 9: 149-158. Tripathi M, Tang CC, Feigin A, et al. Automated Differential Diagnosis of Early Parkinsonism using Metabolic Brain Networks: A Validation Study. J Nucl Med 2016; 57: 60-66.
To cite this abstract in AMA style:
K. Schindlbeck, D. Gupta, C. Tang, S. O'Shea, K. Poston, V. Dhawan, J.P Vonsattel, S. Fahn, D. Eidelberg. Automated pattern based classification in neuropathology proven parkinsonism [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/automated-pattern-based-classification-in-neuropathology-proven-parkinsonism/. Accessed April 26, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/automated-pattern-based-classification-in-neuropathology-proven-parkinsonism/