Session Information
Date: Wednesday, June 7, 2017
Session Title: Myoclonus
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To present the first case series of asymmetric orthostatic myoclnus and its reversibility along with the improvement of the underlying disease
Background: Orthostatic myoclonus (OM) is a syndrome with irregular muscle bursts ranging from 20 to 100ms upon standing. It is secondary to neurodegenerative diseases or peripheral lesions, such as arthritis. All previous studies describe symmetric myoclonic jerks of both legs while asymmetric OM has not been reported.
Methods: Three cases of asymmetric OM were reported. One was secondary to Parkinson disease and the rest were due to lumbosacral radiculopathy.
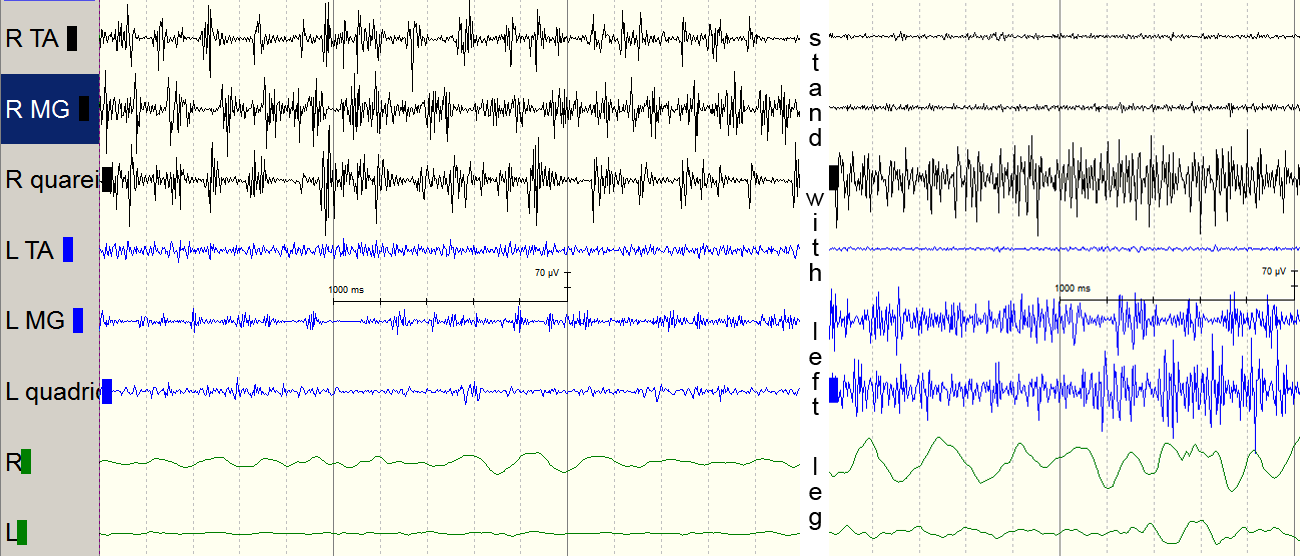
Results: Case 1 was an 85-year-old female with gouty arthritis. She had wobbling gait for 2 years. The nerve conduction study (NCS) and spinal MRI revealed lumbosacral radiculopathy. The tremor study (EMG) showed arrhythmic, 50-100ms bursting activity of the right tibialis anterior (TA), gastrocnemius (MG), and rectus femoris muscles. Standing with the left leg did not show similar finding [figure1].
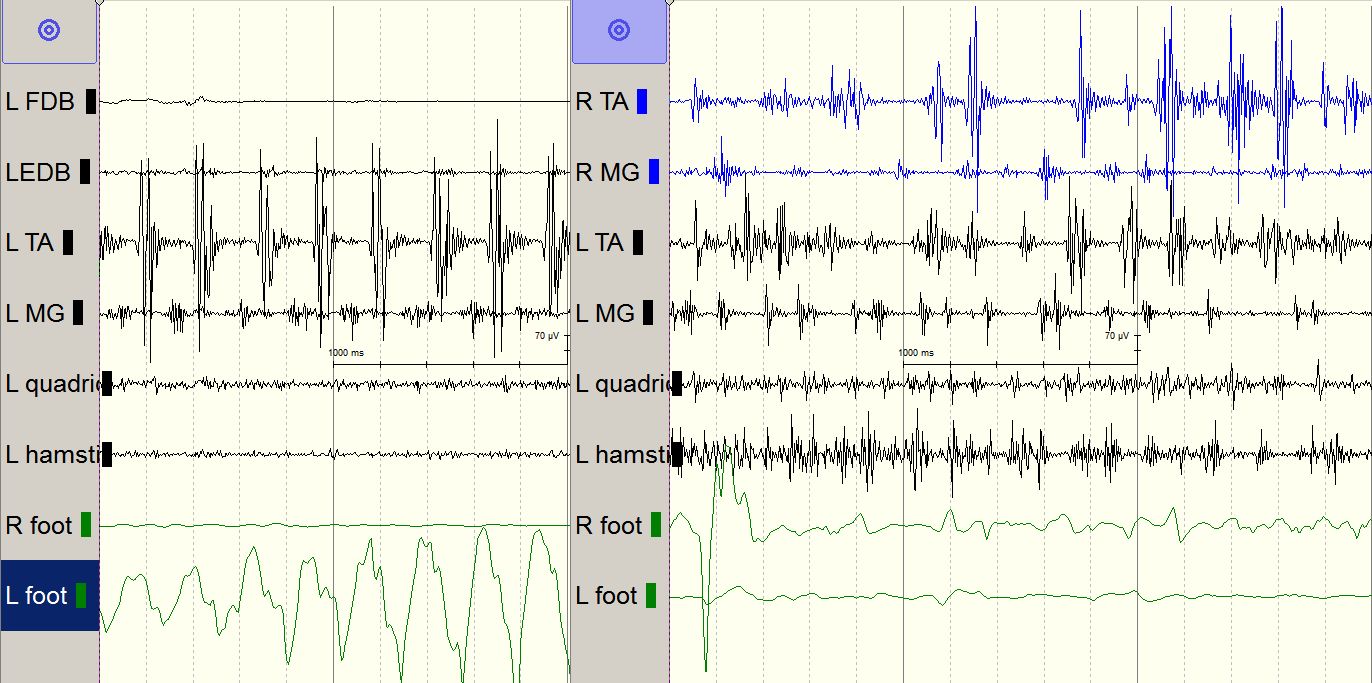
Case 2 was a 68-year-old female with end stage renal disease. She had left leg resting tremor for 2-3 years which improved with standing or walking. She did not have unsteadiness or falling. EMG revealed a 4Hz parkinsonian tremor of the left foot with alternating bursting of TA and MG. During standing, the bursting activity became irregular in frequency (4-7Hz) and duration (50-100ms), mainly involving the left leg. Similar findings were not detected while legs were outstretched without weight bearing [figure2]. TRODAT confirmed the Parkinson disease.
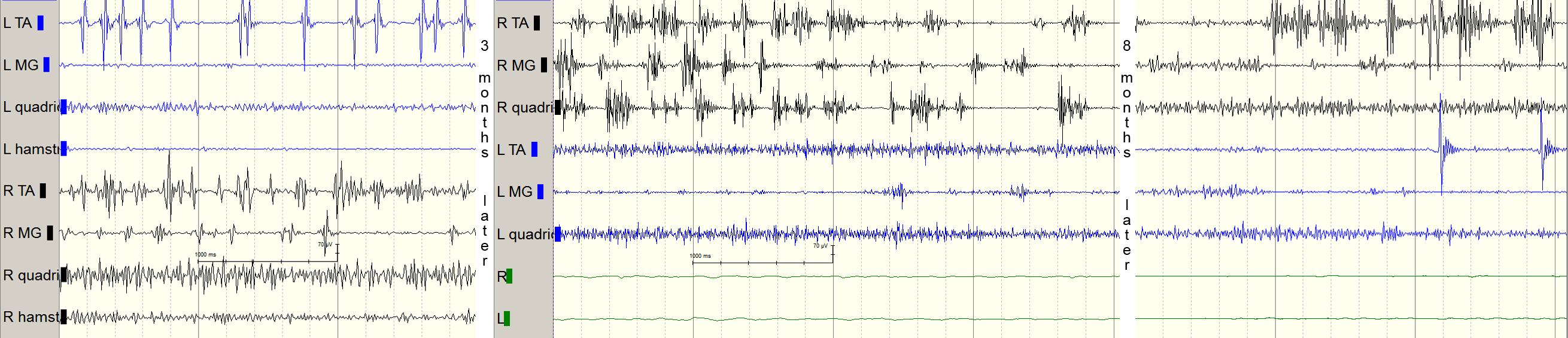
Case 3 was a 58-year-old female with DM. She had unsteadiness during standing for 6 months without falling, which aggravated after the cessation of hypnotics. The NCS and spinal MRI illustrated lumbosacral radiculopathy. EMG showed irregular and 20-100ms bursting activity of bilateral TA and the right MG. She was treated with physiotherapy, mecobalamine, and clonazepam. Three month later, the bursting activity was confined to the right leg. Eight more months later when she felt a significant improvement, there was a complete resolution of OM on EMG [figure3].
Conclusions: OM is a dynamic syndrome and the asymmetry may indicate its immaturity. The bursting duration of myoclonic jerks remained within 100ms even of peripheral cause, which imply the nervous system lesion is the trigger but not the origin of the myoclonus. Our case 3 demonstrates the reversibility of the OM after the removal of the triggering element.
References: 1. Orthostatic myoclonus: A contributor to gait decline in selected elderly. Glass GA, Ahlskog JE, Matsumoto JY. Neurology. 2007 May 22;68(21):1826-30
2. Four cases of orthostatic myoclonus. Z. Aldaajani et al. J Clin Neurosci. 2016 Jul;29:180-2.
To cite this abstract in AMA style:
Y.-c. Tai, J.-c. Tsou, S.-P. Hsu. Asymmetric Orthostaic Myoclonus – A Case Series [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/asymmetric-orthostaic-myoclonus-a-case-series/. Accessed December 2, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/asymmetric-orthostaic-myoclonus-a-case-series/