Objective: The aim of the study was to evaluate the effects of an aquatic intervention program on ventilatory, gait, daily living activity (ADL) and motor parameters in people with PD.
Background: In Parkinson’s disease (PD) there are respiratory limitations, as well as reduced mobility and physical activity [1]. Physical therapy can act in the prevention and rehabilitation of these ventilatory parameters [2,3], as aquatic physiotherapy has been shown to be beneficial in this population [4].
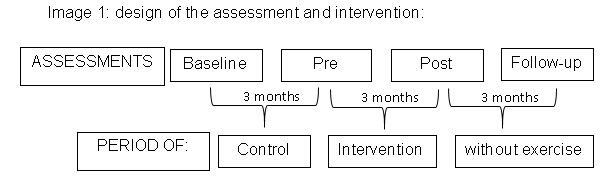
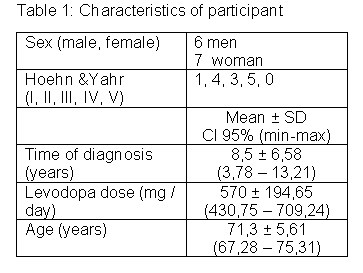
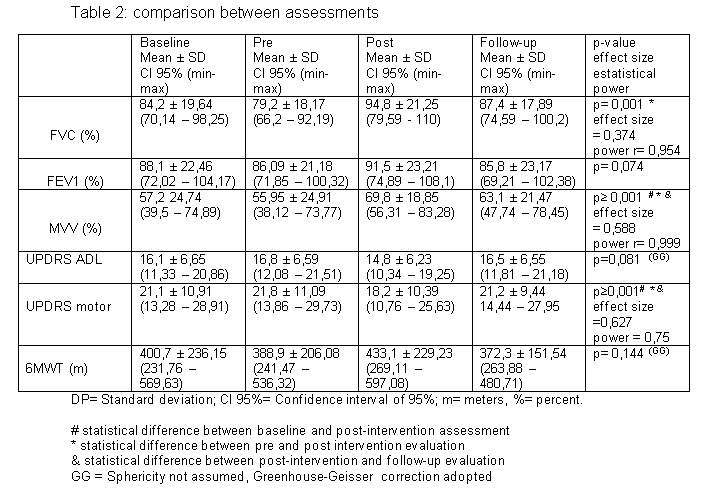
Method: This is a quasi-experimental study, blind evaluator and convenience sampling. The research followed Brazil’s ethics and health guidelines. Participants were recruited from an association in the city of Curitiba, in southern Brazil. Inclusion criteria were both sexes; diagnosis of idiopathic PD in stages 1 to 4 at Hoehn & Yahr; clinical certificate for aquatic physical activity. Exclusion criteria were: no independent gait; disease that could interfere with assessments (eg sensory, visual or auditory deficit, respiratory diseases); absence in more than 10% of the intervention; change in levodopa prescription during study. The evaluations took place in 4 moments, as shown in Image 1. They were evaluated by a six-minute walk test (6MWT), ADL and motor by UPDRS and spirometry: forced vital capacity (FVC); Forced expiratory volume in 1 second (FEV1); Maximum voluntary ventilation (MVV). The interventions took place in a heated pool at 33ºC in 24 meetings over 3 months, twice a week, for fifty minutes each meeting. Each session consisted of warm-up, specialized therapeutic exercises, organic conditioning global and cool down finishing [5]. Exercises based on the five phases of aquatic motor learning were proposed [6]. Data were compared by repeated measures ANOVA. Respiratory variables were analyzed by the percentage of provided for each person [7].
Results: Thirteen patients participated in the aquatic intervention with data and variables shown in Tables 1 and 2. The FVC, MVV and UPDRS motor obtained significative results after 3 months of intervention with Aquatic Physiotherapy. However, after 3 months without exercise the MVV and UPDRS motor returned to the initial parameters.
Conclusion: Aquatic intervention program showed improvement in ventilatory and motor parameters in people with PD.
References: [1] TORSNEY, K. M.; FORSYTH, D. Respiratory dysfunction in Parkinson’s disease. J R Coll Physicians Edinb. v. 47, n.1, p.35-39, 2017. [2] LAMOTTE, G.; RAFFERTY, M. R.; PRODOEHL, J.; KOHRT, W. M.; COMELLA, C. L.; SIMUNI, T.; CORCOS, D. M. Effects of Endurance Exercise Training on The Motor and Non-Motor Features of Parkinson’s Disease: A Review. Journal of Parkinson’s Disease. n. 5, p. 21–41, 2015. [3] BAILLE, G.; JESUS, A. M.; PEREZ, T.; DEVOS, D.; DUJARDINA, K.; CHARLEY, C. M.; DEFEBVRE, L.; MOREAU, C. Ventilatory Dysfunction in Parkinson’s Disease. Journal of Parkinson’s Disease. n. 6, p. 463–471, 2016. [4] TERRENS, A. F.; SOH, S.; MORGAN, P. E. The efficacy and feasibility of aquatic physiotherapy for people with Parkinson’s disease: a systematic review. Pages 2847-2856. Journal Disability and Rehabilitation. v. 40, 2018. [5] KEUS, S. H. J.; MUNNEKE, M.; GRAZIANO, M. et al. European Physiotherapy Guideline for Parkinson’s Disease. 1 ed. KNGF/ParkinsonNet, The Netherlands, dez., 2014. [6] ISRAEL, V. L.; PARDO, M. B. L. Hydrotherapy: a teaching program to develop aquatic motor skills of injured spinal cord in thermal pool. rev. Fisioter. Mov. n.1, v.13, p. 111-127, abr-set., 2000. [7] PEREIRA, C. A. C. Espirometria. J Pneumol v. 28, n. 3, out., 2002.
To cite this abstract in AMA style:
V.L Israel, A. Silva, B. Yamaguchi. Aquatic Physiotherapy increases ventilatory parameters in Parkinson’s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/aquatic-physiotherapy-increases-ventilatory-parameters-in-parkinsons-disease/. Accessed April 21, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/aquatic-physiotherapy-increases-ventilatory-parameters-in-parkinsons-disease/