Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: To describe and correlate the apathy and cognitive profile of patients with Parkinson’s disease (PD).
Background: Prevalence of apathy in PD is highly variable across studies (13.9 to 70%) (1). Some authors suggest that PD apathetic patients had significantly worse neurocognitive performance, higher MDS-UPDRS scores and more severe depressive symptoms (2,3). Although there is a relationship between cognitive performance and apathy, little is known about the interaction between cognitive domains and this symptom.
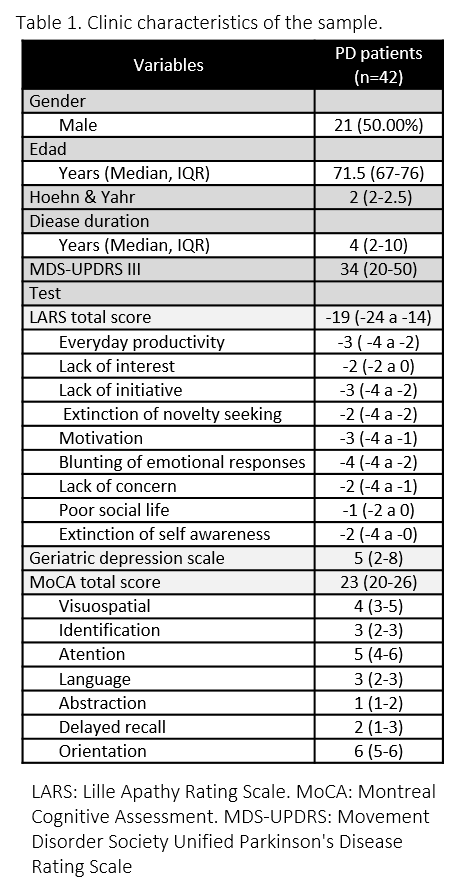
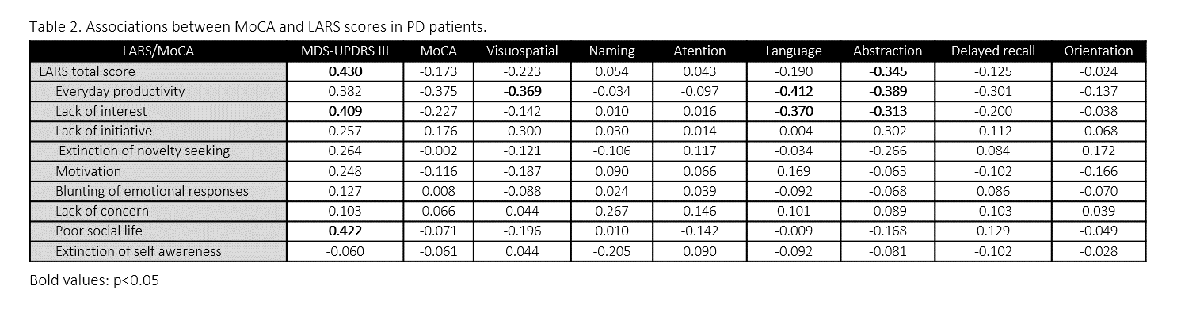
Method: Forty two patients with PD were recruited for the study. Global cognition was evaluated using MoCA test. Apathy and depression were characterized using the Lille apathy rating scale (LARS) and the Geriatric Depression Scale de Yesavage (GDS), respectively. Spearman’s rank correlation was used to correlate the MDS-UPDRS part III, LARS and MoCA test sub scores, Mann Whitney and Chi-squared test were used for comparison between apathetic and non-apathetic PD patients. Statistically significant difference was considered if the p-value was lower than 0.05.
Results: Median duration of the disease from onset was 4 years (IQR 2-10). MDS-UPDRS part III mean was (±13.74) [table 1]. Mean MoCA test score was 23 (20-26), 17 (40.47%) patients had mild cognitive impairment (MCI). Mean LARS score was -19 (ICR -24 to -14), apathy was present in 38.09% (17) of PD patients. Mean Yesavage score was 5 (ICR 2-8). A significant positive correlation was found between the MDS-UPDRS and: the LARS total score (0.430 p=0.004) and intellectual curiosity (0.409 p=0.007) LARS sub score. Significant negative correlations were found between LARS daily productivity and the visuospatial (-0.369 p=0.016) and language (-0.412 p=0.007) MoCA domains; and between LARS intellectual curiosity and the language domain (-0.370 p=0.016) from MoCA test. No significant correlations were found between MoCA total score and the LARS sub scores.
Conclusion: There is a correlation between apathy and the cognitive and motor profile in patients with PD. Visuospatial and language deficiencies are related to the restrictions of daily productivity, probably due to the restriction in the execution of task that depends on frontal lobe functions. The highest scores of MDS-UPDRS are related to a poor social life these could be related to mobility limitations. Apathy should be assessed to complement the motor and cognitive evaluation of PD patients.
References: 1. Santangelo G, Trojano L, Barone P, Errico D, Grossi D, Vitale C. Apathy in Parkinson’s disease: diagnosis, neuropsychological correlates, pathophysiology and treatment. Behav Neurol. 2013 Jan 1;27(4):501–13. 2. Weintraut R, Karádi K, Lucza T, Kovács M, Makkos A, Janszky J, et al. Lille Apathy Rating Scale and MDS-UPDRS for Screening Apathy in Parkinson’s Disease. J Parkinsons Dis. 2016;6(1):257–65. 3. Sousa M, Moreira F, Jesus-Ribeiro J, Marques I, Cunha F, Canário N, et al. Apathy Profile in Parkinson’s and Huntington’s Disease: A Comparative Cross-Sectional Study. Eur Neurol. 2018;79(1–2):13–20.
To cite this abstract in AMA style:
B. Muñoz, J. Valderrama, L. Botero, J. Orozco. Apathy and cognitive profile in Parkinson´s disease: A cross-sectional study in Cali-Colombia [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/apathy-and-cognitive-profile-in-parkinsons-disease-a-cross-sectional-study-in-cali-colombia/. Accessed February 14, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/apathy-and-cognitive-profile-in-parkinsons-disease-a-cross-sectional-study-in-cali-colombia/