Session Information
Date: Monday, June 5, 2017
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: Report a case of rapidly progressive dementia and parkinsonism related to gliomatosis cerebri.
Background: Neoplasms may present as parkinsonian syndrome due to impairment of thalamocortical pathway or nigrostriatal structures, mainly by compression. Moreover, there are few reports of neoplastic parkinsonism secondary to infiltrative gliomas, especially those presenting as gliomatosis cerebri.
Methods: Case report.
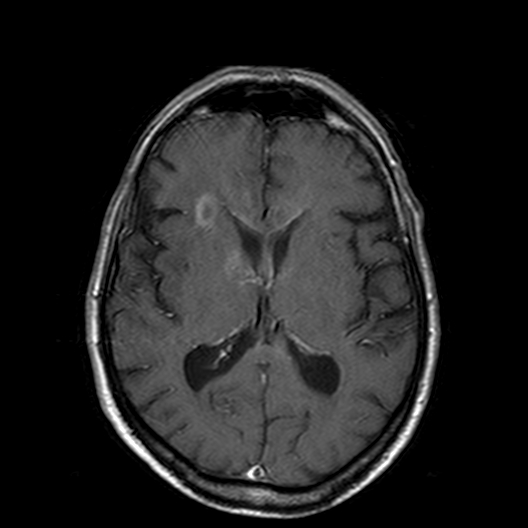
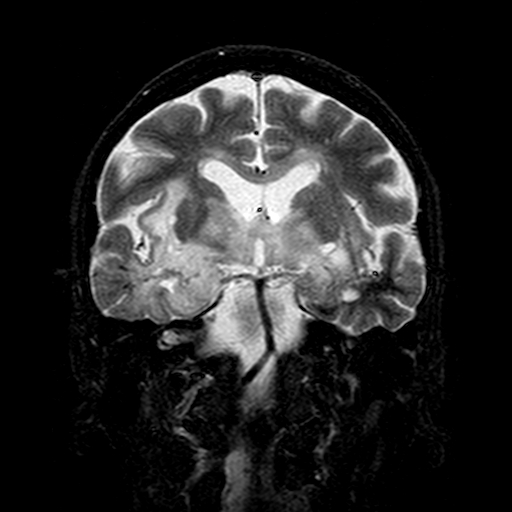
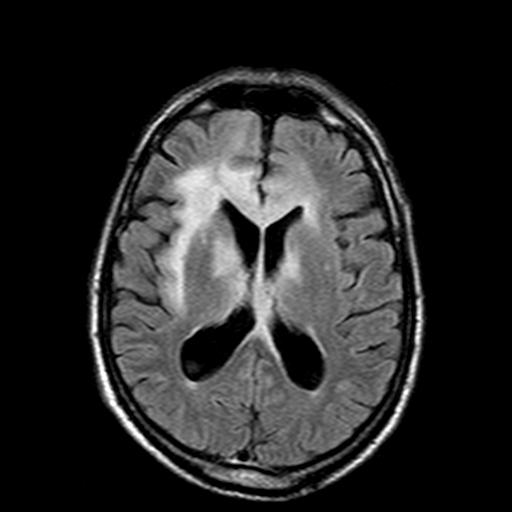
Results: 77 year-old male reported a three-year history of progressive and asymmetric non-levodopa responsive parkinsonism with gait difficulties, early postural instability and frequent falls, dysphagia and cognitive impairment. He had both short and long-term memory loss associated with marked personality changes, with fluctuating cognition. There was no history of seizures, hyposmia, constipation, sleep disturbances and hallucinations. Past medical history was significant for depression, anxiety and hypertension, for which he took imipramine, clonazepam and hydrochlorothiazide. On examination, he exhibited facial hypomimia, upward gaze limitation, hypophonia and asymmetrical rigid-akinetic parkinsonism (worse on left). He scored 26 out of 30 points in the Mini-Mental State Examination. There was no evidence of orthostatic hypotension or pyramidal tract dysfunction. Brain MRI showed white matter hyperintensity on T2/FLAIR and iso/hypointensity on T1 that involved temporal lobes, insula, hippocampal and parahippocampal regions, straight and superior frontal gyrus, besides the knee of the corpus callosum, basal ganglia and thalamus (Figure 1 and 2) . There were also nodular formations on the knee of the corpus callosum and nucleocapsular regions that exhibited annular enhancement after gadolinium injection (Figure 3). An open brain biopsy was performed and the patient was diagnosed with diffuse glioma. Due to clinical, radiological and pathological findings, the patient was diagnosed with a rare pattern of glioma growth and infiltration, previously defined as gliomatosis cerebri.
Conclusions: Gliomatosis cerebri may rarely present with parkinsonism and must be consider in the differential diagnosis of atypical parkinsonian disorders, especially those manifesting with rapidly progressive cognitive decline, epilepsy or elevated intracranial pressure syndrome.
References: Duron E, Lazareth A, Gaubert JY, Raso C, Hanon O, Rigaud AS (2008) Gliomatosis cerebri presenting as rapidly progressive dementia and parkinsonism in an elderly woman: a case report. Journal of medical case reports.2:53.
Greenfield JP, Castaneda Heredia A, George E, Kieran MW, Morales La Madrid A (2016) Gliomatosis cerebri: A consensus summary report from the First International Gliomatosis cerebri Group Meeting, March 26-27, 2015, Paris, France. Pediatric blood & cancer.63(12):2072-7.
To cite this abstract in AMA style:
H. Oliveira, P. Oliveira, V. Calil, P. Macêdo, N. Canedo, L. Vasconcellos. An unusual mimicker of Lewy Body Dementia: Gliomatosis Cerebri. [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/an-unusual-mimicker-of-lewy-body-dementia-gliomatosis-cerebri/. Accessed April 25, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/an-unusual-mimicker-of-lewy-body-dementia-gliomatosis-cerebri/