Category: Choreas (Non-Huntington's Disease)
Objective: Our aim is to shed light on an usual cause of choreoathetosis in a medically complex case.
Background: Goodpasture’s syndrome(GBS) is a rare autoimmune disease. Typical manifestations include pulmonary-renal syndromes secondary to anti-glomerular basement membrane(GBM) antibody deposition. CNS involvement is rarely reported. We present a case of a gentleman with a recent diagnosis of GBS presenting with choreoathetosis and a generalised tonic-clonic seizure.
Method: A 60-year old smoker, hypertensive gentleman, was diagnosed with GBS-renovasculitis 3-months prior admission following investigations for nephrotic syndrome. He had presented to Nephrology with a 3-month history of decreased exercise tolerance, oliguria and lethargy. 24-hour urine protein collection confirmed nephrotic syndrome [protein 1.5g/day]. A vasculitis work up revealed an elevated anti-GBM titre. The patient was given a 3-day course of IV MTP and required indefinite renal replacement therapy due to refractory hyperkalaemia and anuria.
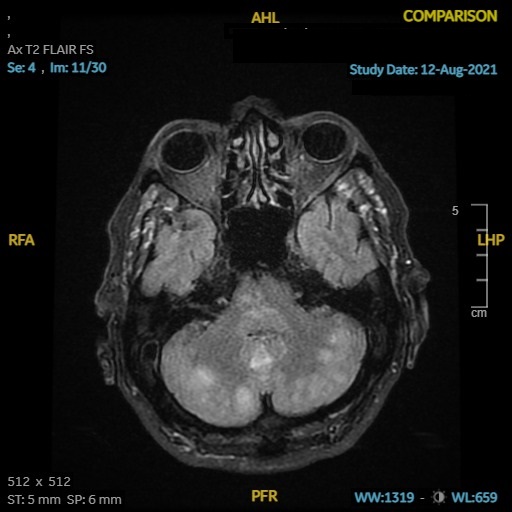
2-months following diagnosis, the patient was admitted with a generalised tonic-clonic seizure. He was noticeably hypertensive and had choreiform movements affecting his lower extremities. A petechial non-blanching rash was also noted. He was started on anti-epileptic medications. An EEG and CSF were unremarkable [table 1]. An MRI revealed patchy areas of T2 signal change affecting bilateral cerebellar hemispheres, parietal, and occipital lobes [figure 1]. Non-specific arterial beading within the right M1, bilateral M2 and left P1 was noted. A diagnosis of anti-GBM CNS vasculitis vs posterior reversible encephalopathy syndrome (PRES) was suspected. He was given 4 cycles of plasma exchange and later started on cyclophosphamide 50mg daily for a presumed anti-GBM vasculitis.
He improved clinically and biochemically. Choreiform movements subsided significantly after 4 days. An MRI which was repeated after 6 days showed resolution of the T2 change [figure 2]. Beading on MRA was no longer appreciated. The rapid resolution of MR Angiography changes made the diagnosis of PRES more likely. Cyclophosphamide was eventually stopped.
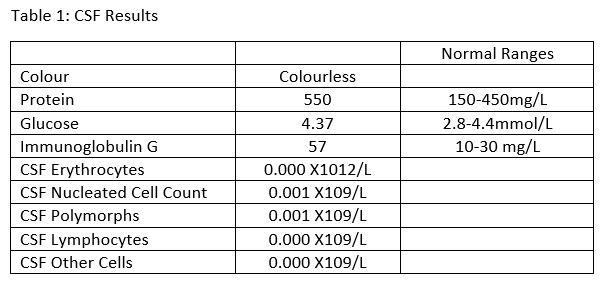
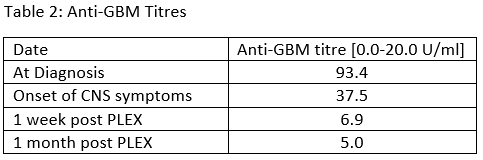
Results: [table 1]
[table 2]
Conclusion: This case sheds light on an uncommon cause of chorea-athetosis in a patient suffering from PRES in the setting of a rare renovascular disease such as Goodpasteur’s syndrome. It also shed light on the diagnostic dilemma of differentiating PRES form cerebral vasculitis.
To cite this abstract in AMA style:
M. Bonello, M. Cauchi, R. Debono, N. Vella. An unusual cause of choreoathetosis: PRES and Goodpasture’s Syndrome [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/an-unusual-cause-of-choreoathetosis-pres-and-goodpastures-syndrome/. Accessed February 21, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/an-unusual-cause-of-choreoathetosis-pres-and-goodpastures-syndrome/