Category: Parkinson's Disease: Neuroimaging
Objective: Virus related Parkinsonism causing encephalitis lethargica has been documented in the literature. The novel Coronavirus (COVID-19) has been linked to a small number of cases of Parkinsonism.
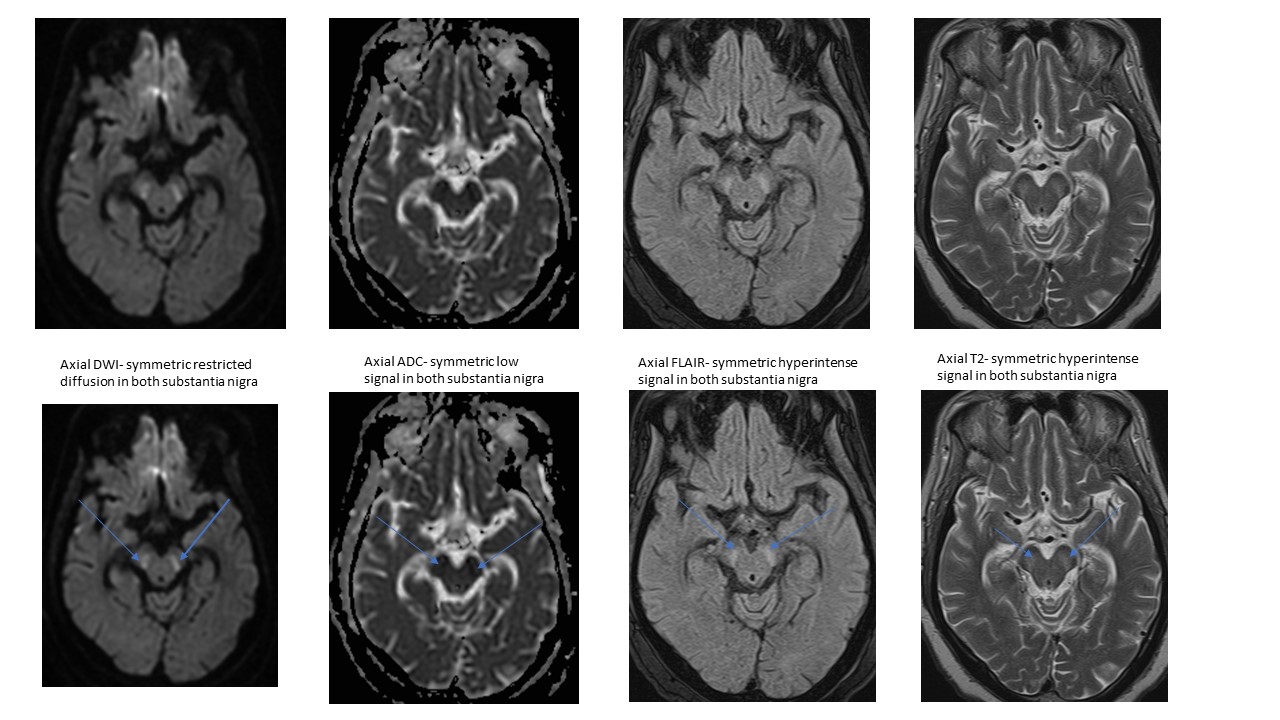
Background: A 58-year-old man was admitted with acute respiratory distress after a grade 4 COVID-pneumonia.His medical history was significant for dyslipidemia, uncontrolled insulin-dependent Diabetic Mellitus, and hypertension.Standard of care for COVID-19 was started, including Dexamethasone, Remdesivir, Tocilizumab, and prone positioning.Even with maximum non-invasive ventilation, the patient was unable to tolerate prone positioning, necessitating intubation using Nimbex.Additional pressor support became imperative when his clinical state deteriorated.His hospital course was further complicated by Methicillin Sensitive Staphylococcus aureus (MSSA) bacteremia, septic shock, atrial fibrillation, acute renal damage, and eventually a Percutaneous Endoscopic Gastrostomy (PEG) tube.15 days later, he experienced sudden change in mentation and a high-grade fever.His extremities were flaccid (0/5 motor strength in all extremities) and developed a gaze deviation.A CT head did not show any acute findings.At this point, a neurology consultation was requested.He was diagnosed with locked-in syndrome with an uncertain origin.Possibility of seizure was also thought of; thus, he was trialed on Ativan and Keppra with no improvement in gaze.An electroencephalogram revealed a continuous slow generalization without any epileptiform discharges.MRI of the brain showed diffusion restriction in the bilateral substantia nigra of the midbrain (Figure. 1).This diagnostic conundrum led to a lumbar puncture, revealing an increased protein (72 mg/dL) but, otherwise, nonspecific. His clinical picture and radiological findings aroused suspicion of Parkinson-like syndrome. A Sinemet trial was started at a dose of 25 mg/100 mg three times daily (TID), up-titrated per response. This showed significant clinical improvement in his motor and non-motor symptoms. Throughout his hospital stay, he continued to advance in his medical condition. Subsequently, he was discharged with physiotherapy and a maintenance Sinemet 50/200 mg dosing schedule.
Method: NA
Results: NA
Conclusion: In a predisposed individual, COVID-19 illness can result in parkinsonism. To ascertain if the impact on dopaminergic activity is short-term or long-lasting, more research is required.
To cite this abstract in AMA style:
P. Bhatia, A. Ata, K. Bailey. An Interesting Case of COVID-19 related Parkinsonism [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/an-interesting-case-of-covid-19-related-parkinsonism/. Accessed April 20, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/an-interesting-case-of-covid-19-related-parkinsonism/