Session Information
Date: Saturday, October 6, 2018
Session Title: Clinical Trials and Therapy in Movement Disorders
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: We explored the efficacy and neural mechanisms of repetitive transcranial magnetic stimulation (rTMS) over the supplementary motor area (SMA) on freezing of gait (FOG) in Parkinson’s disease (PD).
Background: FOG contributes to falls and greatly reduced mobility in PD, however, robust effective treatments remain elusive.
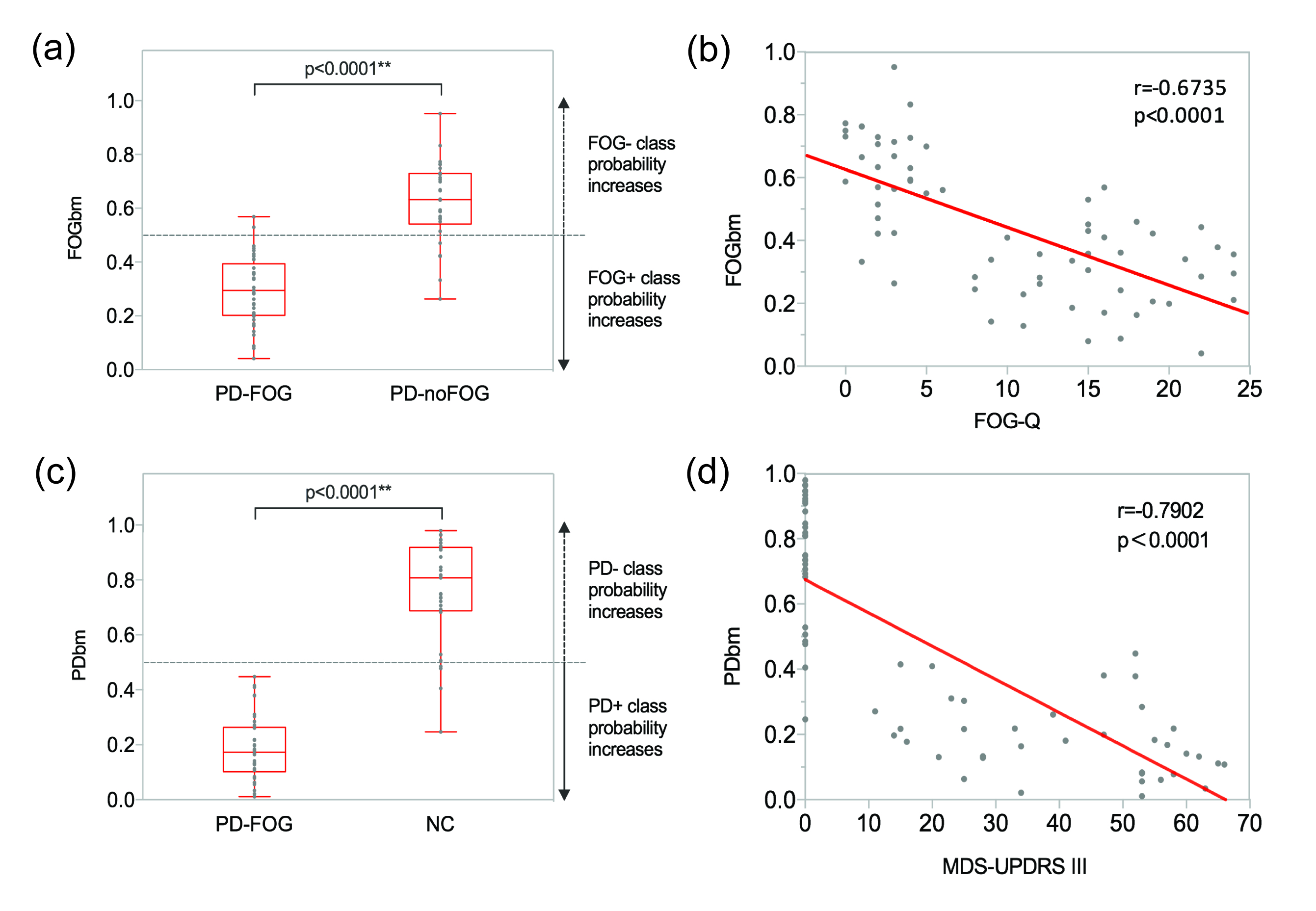
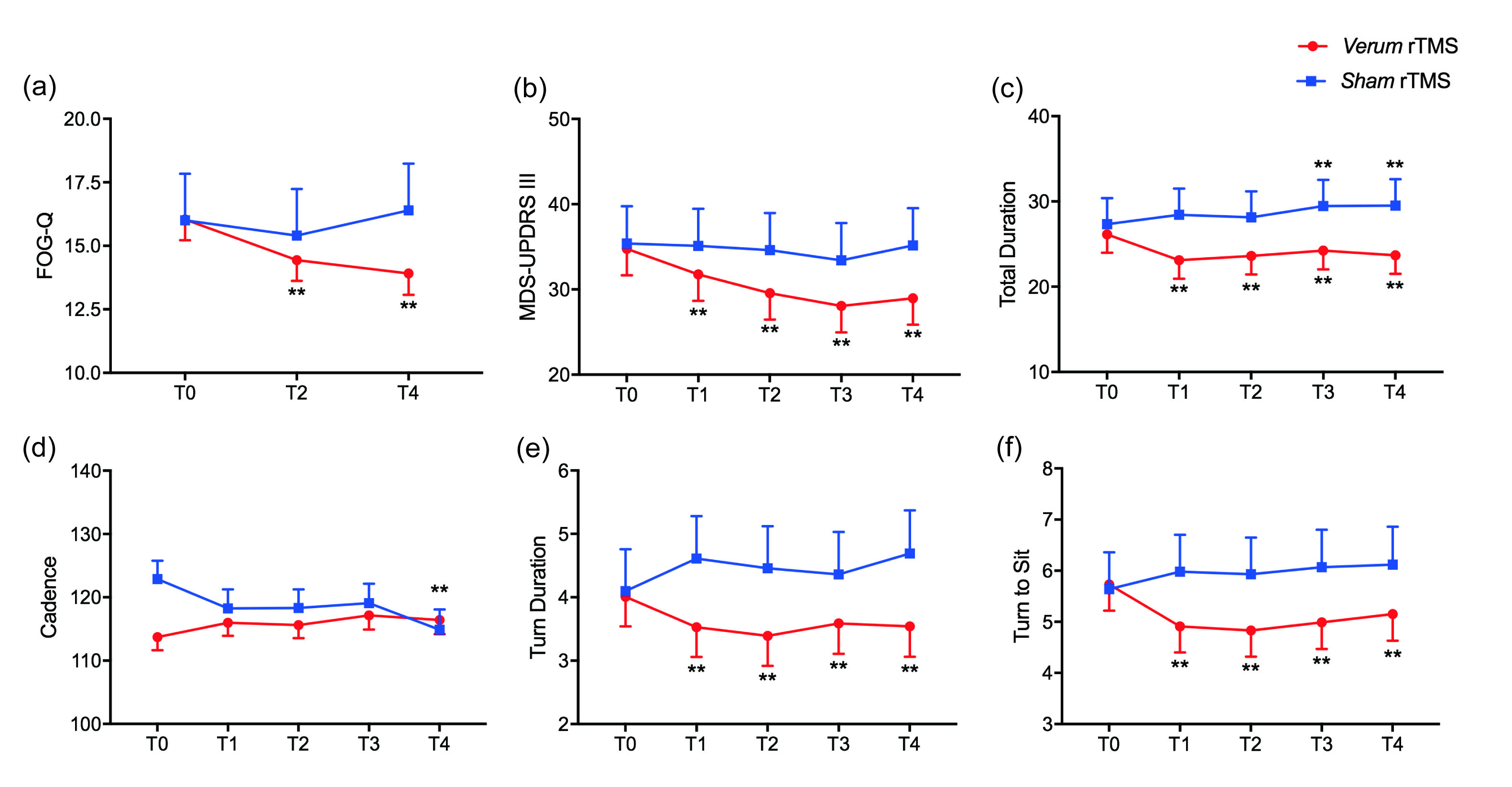
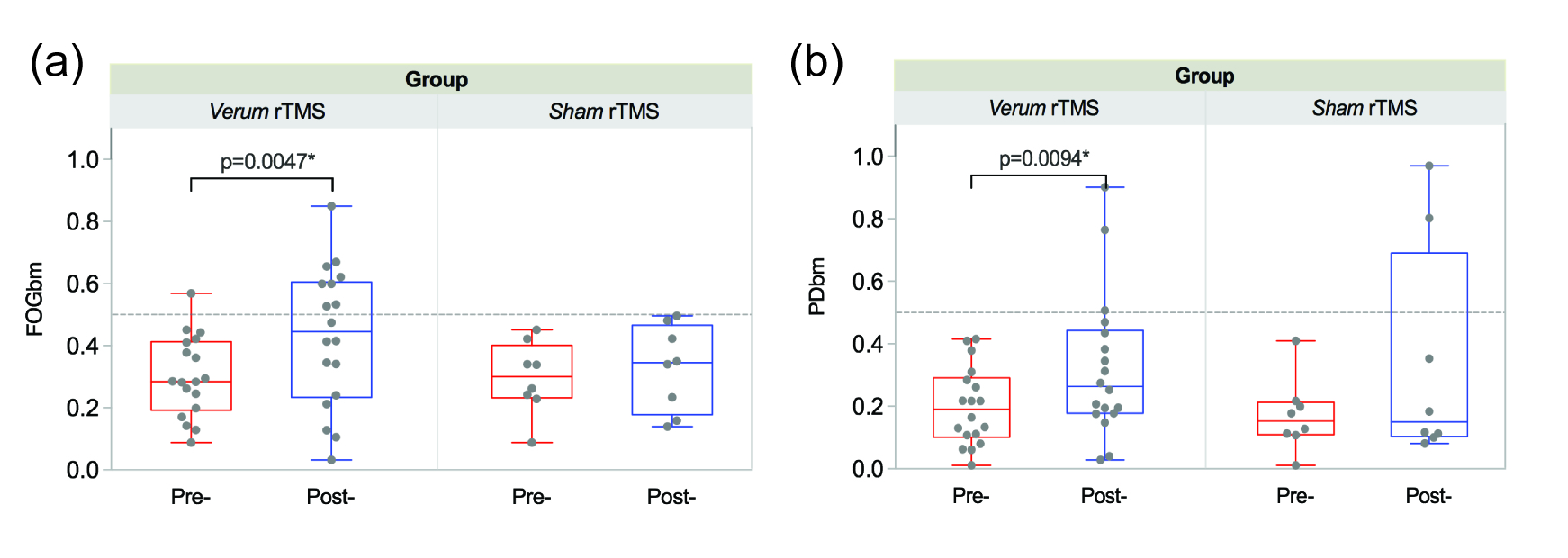
Methods: We first conducted a resting-state fMRI (rs-fMRI) study using a group of 40 PD patients with FOG (PD-FOG), 31 without FOG (PD-noFOG) and 30 normal controls (NC). A subset of 30 PD-FOG participated in a randomized, double-blind, sham-controlled trial to investigate the effects of rTMS on FOG. Patients were randomly assigned (with 2:1 allocation) to receive ten sessions of either verum or sham 10 Hz rTMS over SMA. The primary clinical outcome was the Freezing of Gait Questionnaire (FOG-Q). The Movement Disorder Society Unified Parkinson’s Disease Rating Scale motor score (MDS-UPDRS III) and Timed Up and Go test were secondary clinical outcomes. Rs-fMRI studies were performed at baseline and after the rTMS sessions off medication. The functional connectivity between 48 ROIs that included the fronto-parietal network, frontostriatal loop, and locomotor network were assessed with a Bayesian network methodology. We used the baseline scans to create imaging biomarkers for FOG (FOGbm) and PD (PDbm) by using logististic Least Absolute Shrinkage and Selection Operator regression applied to the rs-fMRI connectivity profiles, and contrasting PD-FOG to PD-noFOG and NC respectively. These biomarkers were then interrogated to assess the effects of rTMS on connectivity patterns.
Results: The FOGbm and PDbm consisted of 14 and 16 functional connections, and included connections to/from the basal ganglia, cerebellar and thalamic regions, precuneus, anterior cingulate cortex, insula cortex and superior temporal gyrus. As anticipated, FOGbm was negatively correlated with FOGQ, and PDbm was negatively correlated with MDS-UPDRS III. After long-term follow-up, significant clinical improvements in FOG-Q, MDS-UPDRS III and several gait variables were found in the verum group. Moreover, both FOGbm and PDbm were significantly improved after verum stimulation. Neither significant clinical improvements nor biomarker changes were found in the sham group.
Conclusions: Our results suggest that high-frequency rTMS over SMA can alleviate FOG in PD through normalizing the abnormal brain functional connectivity patterns of PD-FOG and makes it not only more similar to PD-noFOG, but also more similar to NC.
To cite this abstract in AMA style:
T.M. Mi, S. Garg, F. Ba, T. Wu, P.P. Liang, L.L. Gao, K.C. Li, P. Chan, M. McKeown. Alleviation of freezing of gait in patients with Parkinson’s disease by high-frequency rTMS over SMA is associated with normalization of brain connectivity patterns [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/alleviation-of-freezing-of-gait-in-patients-with-parkinsons-disease-by-high-frequency-rtms-over-sma-is-associated-with-normalization-of-brain-connectivity-patterns/. Accessed January 1, 2026.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/alleviation-of-freezing-of-gait-in-patients-with-parkinsons-disease-by-high-frequency-rtms-over-sma-is-associated-with-normalization-of-brain-connectivity-patterns/