Objective: Given the well-known clinical differences and natural history of Parkinson’s disease (PD) according ot patients age, wthis study aims at exploring the different pathophysiological mechanisms underlying PD in patients of different age, independently from disease duration, through CSF biomarkers.
Background: PD is increasingly diagnosed in younger patients, even if it was classically defined as a disease of the elderly [1]. Clinical evidence indicates that PD patients have different progression rates and disease characteristics[2, 3] the older being more cognitively affected and experiencing less motor fluctuations.
Method: Patients with clinically established diagnosis of PD were enrolled at three different sites in Italy (Policlinico gemelli, University of Perugia and Policlinico Tor Vergata). They underwent clinical evaluation through MDS-UPDRS, NMSS and MoCA scales. CSF inflammatory (YKL-409, TREM-2) and neurodegeneration/synaptopathy (A-beta42 and 40, tau, p-tau, sAPP-a and -b, NfL, Ng) biomarkers were analysed.
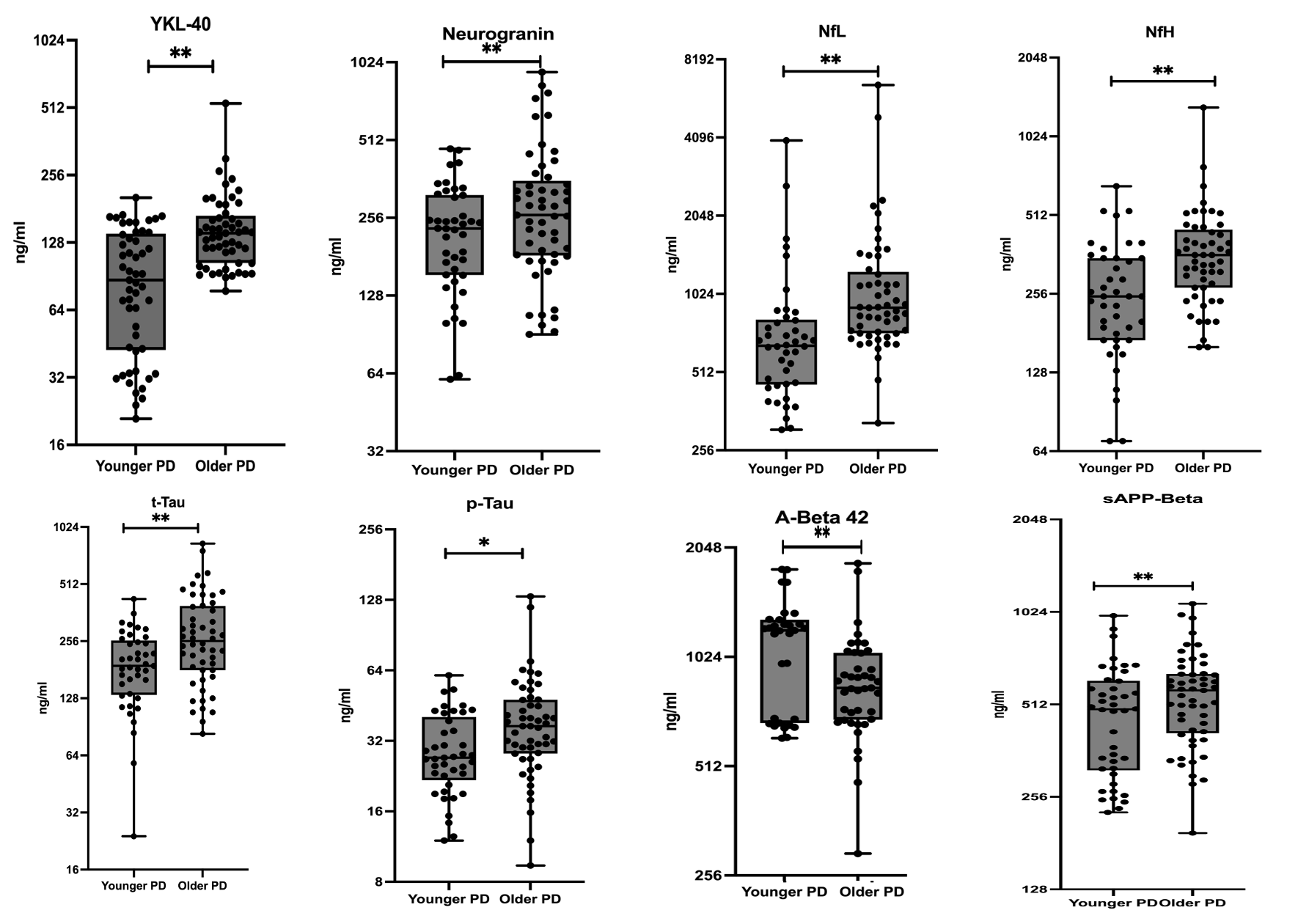
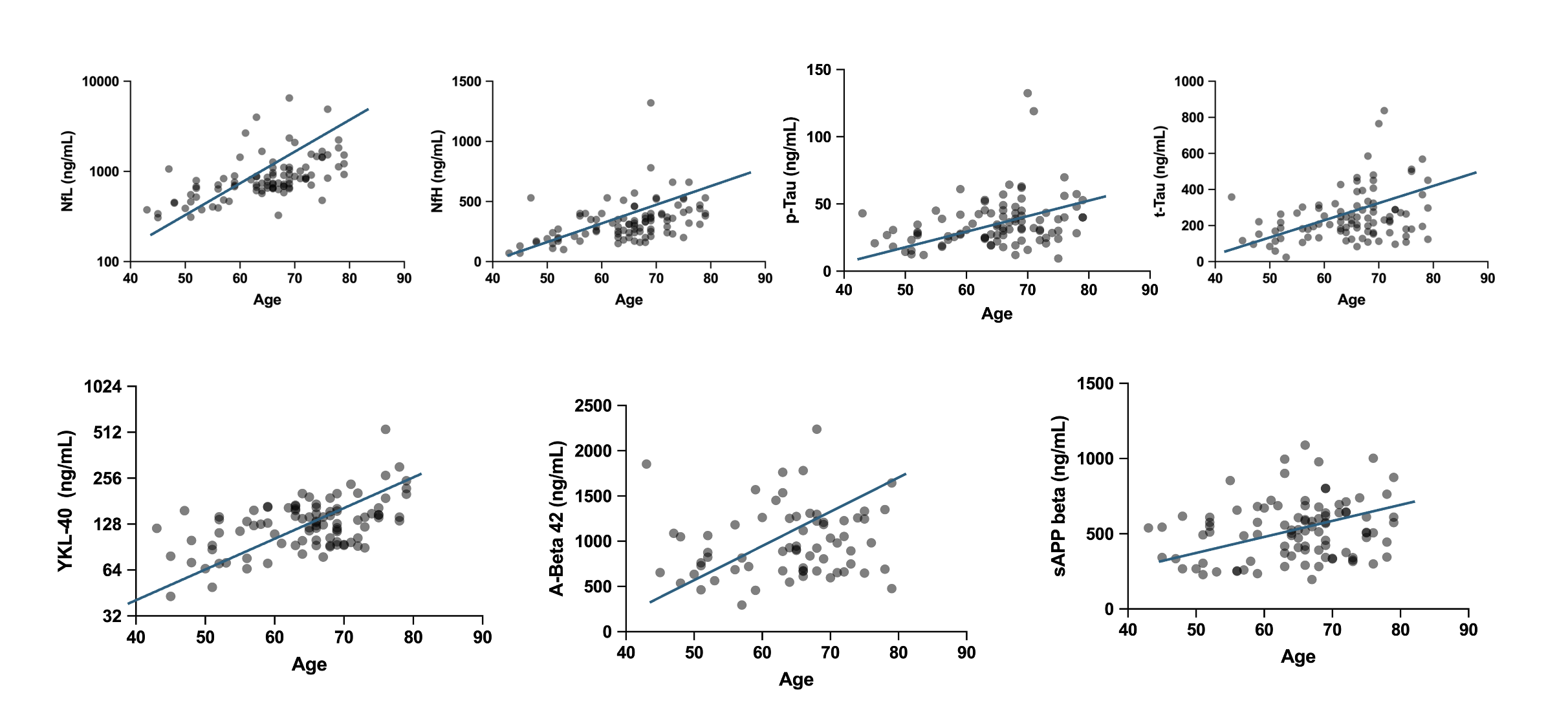
Results: 95 patients were recruited, 42 younger than 65 years-old, and 53 older. Age strongly correlated with NfL CSF levels, with YKL-40 and Alzheimer’s related pathology biomarkers, in a stronger manner with tau species. Younger and older patients showed different biomarkers profile. In particular, younger patients showed significantly lower levels of inflammatory molecules (YKL-40), of degeneration biomarkers (neurogranin, tau species, neurofilaments) and sAPP-beta, independently from disease duration.
From the clinical point of view, younger patients had better scores at UPDRS parts I, II, III and IV and MoCA.
Conclusion: Our data support the hypothesis that PD has different features in younger and older patients, with a different pathology underlying the observed clinical differences. This could reflect a more preponderant loss of integrity of neuronal circuits independently from the nigro-striatal degeneration, as the higher prevalence of amyloid pathology and higher burden of neurodegneration could be related to worse cognitive performances in older patients and lower levodopa-induced dyskinesia, for which an aberrant plasticity is the major recognized pathophysiological mechanism.
CSF biomarkers in younger and older PD
Correlations between CSF biomarkers and age.
References: [1] A. Ascherio and M. A. Schwarzschild, “The epidemiology of Parkinson ’ s disease : risk factors and prevention,” Lancet Neurol., vol. 15, no. 12, pp. 1257–1272, 2016, doi: 10.1016/S1474-4422(16)30230-7.
[2] L. W. Ferguson, A. H. Rajput, and A. Rajput, “Early-onset vs . Late-onset Parkinson ’ s disease : A Clinical-pathological Study,” no. May, pp. 113–119, 2019, doi: 10.1017/cjn.2015.244.
[3] A. W. Willis, M. Schootman, N. Kung, and B. A. Racette, “Epidemiology and neuropsychiatric manifestations of Young Onset Parkinson’s Disease in the United States,” Park. Relat. Disord., vol. 19, no. 2, pp. 202–206, 2013, doi: 10.1016/j.parkreldis.2012.09.014.
To cite this abstract in AMA style:
G. Di Lazzaro, F. Paolini Paoletti, G. Bellomo, T. Schirinzi, P. Grillo, G. Giuffrè, A. Picca, M. Petracca, AR. Bentivoglio, NB. Mercuri, L. Parnetti, P. Calabresi. Age and Parkinson’s disease: clinical and biomarkers profiling of younger and older patients [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/age-and-parkinsons-disease-clinical-and-biomarkers-profiling-of-younger-and-older-patients/. Accessed January 14, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/age-and-parkinsons-disease-clinical-and-biomarkers-profiling-of-younger-and-older-patients/